Improvement in regional disparities in prehospital emergency medical care systems using the prehospital care index: how the timing of adrenaline administration by paramedics impacts cerebral functioning prognosis
Article information
Abstract
Objective
In Japan, the protocol for timing of adrenaline administration by paramedics is determined by the local medical control council. The purpose of this study was to compare, via prehospital care indices, how differences in ‘adrenaline times’ across prefectures influence cerebral functioning prognoses.
Methods
We included 13,326 cases registered in the nationwide Utstein style database. To compare adrenaline administration times and cerebral functioning at 1-month post-event, the average time of adrenaline administration was calculated for each prefecture. A scatter plot showing the correlation of the rating of ‘good’ cerebral function at 1 month, and an approximately linear, were used to review the correlation. All cases where emergency medical technicians administered adrenaline within 10 minutes of field activity were examined bases on the prehospital care index.
Results
The nationwide average adrenaline time was 15.4±6.3 minutes, and the rating of good cerebral outcome at 1 month was 3.0%. 5.4% of good cerebral outcome. The prefecture with the slowest average adrenaline time was Hiroshima, with an average of 19.4±6.4 minutes and a 0.9% good cerebral outcome. Examination between average adrenaline times and good ratings for cerebral outcome at 1 month revealed a negative correlation (R2=0.1295) by prefecture. Aichi prefecture achieved the highest prehospital care index at 75.1%.
Conclusion
Adrenaline administration and the security of intravenous lines should be standardized in practice, with a view to shortening adrenaline administration times, rather than giving adrenaline under on-line medical control.
INTRODUCTION
In Japan, the protocol for the timing of adrenaline administration by paramedics is determined by the local medical control (MC) council of each individual prefecture. The details are accordingly impacted by each local emergency medical system. This has implications for the timing of adrenaline administration.
The effectiveness of early adrenaline administration has recently been confirmed. In 2014, Donnino et al. [1] reported that early adrenaline administration with non-shockable rhythm cardiac arrest patients positively influenced outcomes. The following year, Ewy et al. [2] demonstrated that early adrenaline administration with out-of-hospital cardiac arrest (OHCA) patients significantly improved resuscitation rates. In a Japanese study, Tanaka et al. [3] reported that adrenaline administration within 19 minutes of the 119 call (the Japanese emergency activation number) resulted in improved neurological outcomes.
‘Response time’ is defined as the time between the 119 call and the emergency medical technicians (EMTs) contact with the patient. The national average response time in Japan is currently around 8 minutes. Response times are dependent on local emergency medical systems as well as traffic volumes and are thus difficult to shorten. ‘Adrenaline time,’ however, relates to the time between the initial EMT contact with the patient and adrenaline administration, and this is something that could be shortened by changing protocols.
The purpose of this study was to compare, via prehospital care indices, how differences in adrenaline times across prefectures influence cerebral functioning prognoses.
METHODS
Emergency activity protocols
The protocols for paramedic activity and medical standards are created by the local MC councils. As of 2018, there have been 251 local MC councils, but similar protocols tend to be applied within the same prefecture. The Ethics Committee at Kokushikan University approved this study (No. 16-MJ015). Informed consent and study approval were not taken due to the nature of the study.
Data collection and quality assurance
Utstein style, the national database registry of OHCA, was received from the Fire and Disaster Management Agency (FDMA). Individual details in the data were deleted and anonymized. Upon receiving the information, data cleaning was performed following the usual procedures, details of which can be accessed in the report of March, 2009 [4].
Cerebral function prognoses were measured by the Glasgow-Pittsburg cerebral performance category (CPC) scores (CPC1, good cerebral functioning; CPC2, moderate cerebral disability; CPC3, severe cerebral disability; CPC4, coma or vegetative state; and CPC5, death or brain death). The CPC score measurement was performed by physicians at the hospital to which the patient had been transported [5].
Inclusion criteria and extrication
Our study included 13,326 of 506,046 cases registered on the nationwide Utstein style database between January 1st 2011 and December 31st 2014. Inclusion criteria were (1) aged between 8 and 110 years of age, (2) the cardiac event being witnessed by citizens, (3) a cardiogenic event, (4) adrenaline administered by paramedics. The following 8 conditions comprised the exclusion criteria: (1) the cardiac arrest being witnessed by the EMT crew, (2) advanced life support performed by physicians, (3) the presence of return-of-spontaneous circulation (ROSC) by defibrillation (only one defibrillation being performed on ventricular fibrillation or ventricular tachycardia on the initial electrocardiogram (ECG), and the presence of ROSC being within 4 minutes of the initial defibrillation), (4) the use of pyritize for advanced airway management, (5) the performance of emergency care not inputted in the data, (6) negative value on the time factor, (7) the time factor being an outlier (greater than 99th percentile), and (8) the response time being more than 16 minutes and the time lapse more than 22 minutes after EMTs’ contact with patient (greater than 99th percentile). The reason for excluding response times greater than 16 minutes was that only 5% of all OHCA cases took more than 16 minutes and these would therefore be beyond the scope of this study (Fig. 1).

Flow chart of inclusion and exclusion in the analysis. Response time: the time between the 119 call and the emergency medical technicians (EMTs) contact with the patient. Adrenaline time: the time between the initial EMT contact with the patient and adrenaline administration. ALS, advanced life support, ROSC, return-of-spontaneous circulation; EMS, emergency medical service; CPR, cardiopulmonary resuscitation; PAD, public access defibrillation.
Endpoint
We set the endpoint for each prefecture as a rating of ‘good’ cerebral outcome at 1 month, which is defined by CPC1 and CPC2 on the Glasgow-Pittsburg CPC.
Statistical analysis
To compare adrenaline administration times and cerebral functioning at 1 month postevent, the average time of adrenaline time was calculated for each prefecture. The average adrenaline time was presented as mean and standard deviation because because the data were found to be normality distributed in the normality test. A scatter plot showing the correlation of the rating of good cerebral function at 1 month, and an approximately linear, were used to review the correlation. In most area, emergency medical service (EMS) field activity time is aimed to be within 10 minutes. All cases where EMTs administered adrenaline within 10 minutes of field activity after making contact with the patient were examined, as the prehospital care index. We used Excel 2016 MSO (16.0.9226.2114; Microsoft Corp., Redmond, WA, USA) to calculate the linear regression and a coefficient of determination R2.
RESULTS
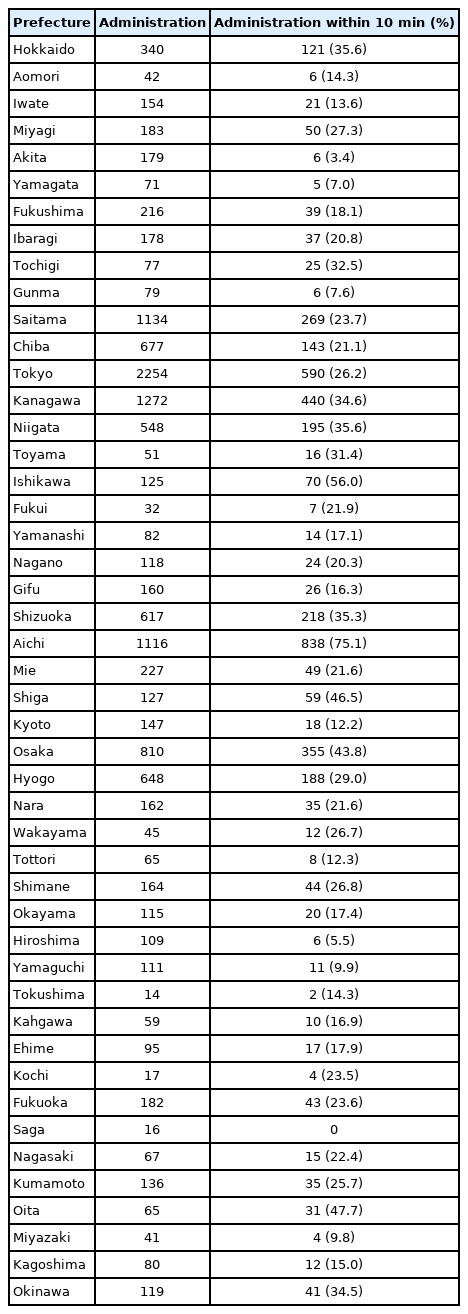
Average of adrenaline time and a rating of good cerebral outcome at 1 month, by prefecture
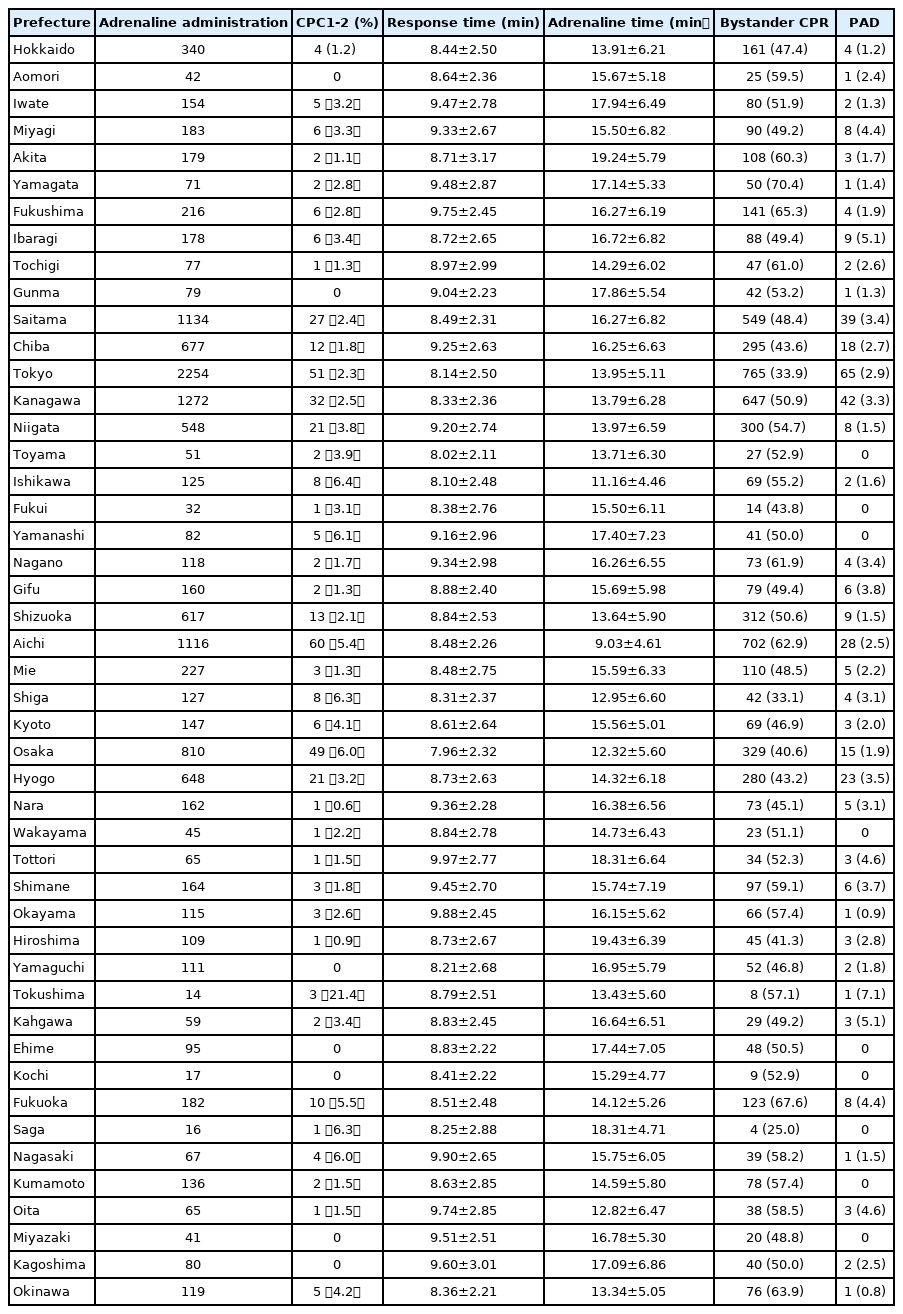
The nationwide average adrenaline time was 15.4±6.3 minutes, and the rating of good cerebral outcome at 1 month was 3.0%. The prefecture with the shortest adrenaline time, Aichi prefecture, averaged 9.0±4.6 minutes and had a 5.4% (60/1,116) good rating for cerebral outcome at 1 month postevent. Aichi was followed by Ishikawa prefecture, which took on average 11.2±4.5 minutes, and which had a 6.4% (8/125) good rating at 1 month. The ‘slowest’ prefecture was Hiroshima, which took 19.4±6.4 minutes and had a 0.9% (1/109) good cerebral outcome rating at 1 month. Tokushima prefecture averaged at 13.4±5.6 minutes and a 21.4% (3/14) good rating. Thus, the result of examining the relation between average adrenaline times and good ratings for cerebral outcome at 1 month, by prefecture, revealed a negative correlation (y=-0.0059x+0.1207, R2=0.1295). The shortest response time was 8.0±2.3 minutes (Osaka prefecture) and the longest 10.0±2.8 minutes (Tottori prefecture) (Fig. 2, Table 1).
The result of examining the relation between mean ‘adrenaline times’ and ‘good’ ratings for cerebral outcome at 1 month, by prefecture.
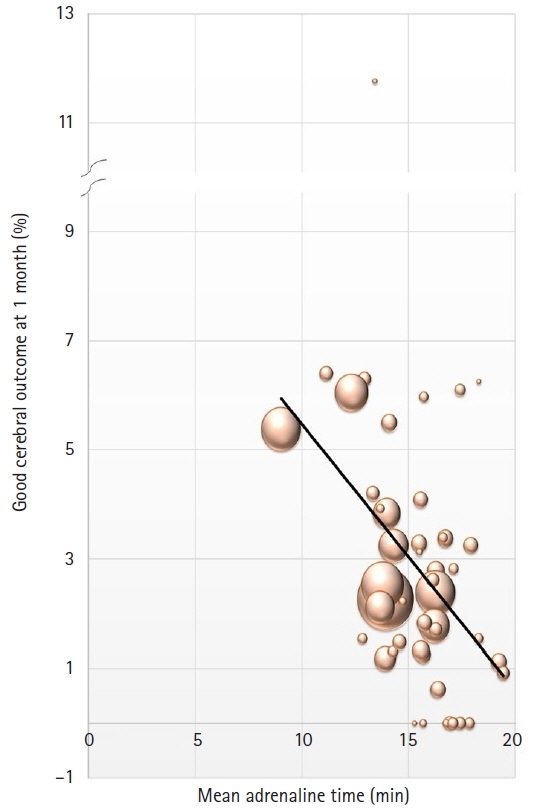
Comparison of the prehospital care index
We defined the ‘prehospital care index’ as the rate of at which adrenaline administration took place within 10 minutes of EMT contact with patients. The highest score in this regard was achieved by Aichi prefecture, at 75.1% (838/1,116), followed by Ishikawa, at 56.0% (70/125), Oita at 47.7% (31/65), Shiga prefecture, Osaka prefecture (Fig. 3, Table 2).
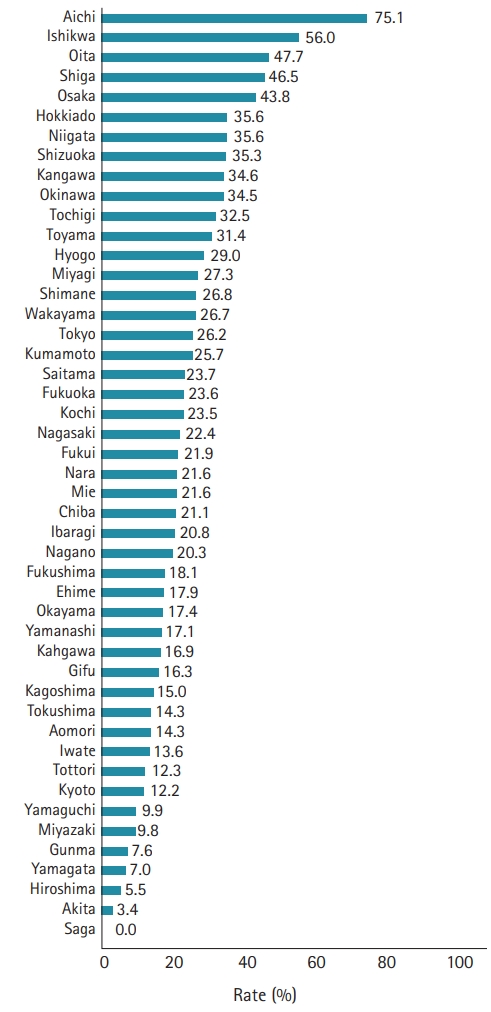
The rate of at which adrenaline administration took place within 10 minutes of emergency medical technician contact with patients.
DISCUSSION
This study has revealed variation in emergency protocols. The highest prehospital care index recorded was 75.1% (838/1,116) (Aichi prefecture), and the second highest was 56.0% (Ishikawa prefecture). These scores were followed by Oita prefecture, Shiga prefecture, and Osaka prefecture. There was also found to be a difference in the time taken to administer adrenaline. This was because the initial adrenaline administration was only permitted before the patient was put into the ambulance or before the ambulance arrived at the hospital.
The protocol for adrenaline administration was seen to vary. In some areas, this followed on-line MC by a physician on each occasion or standard order after the second administration.
The protocol for the shortest adrenaline time, in Aichi prefecture, followed specific timing conditions: securing the intravenous (IV) line within 4 minutes of EMT contact with the patients, giving the initial adrenaline administration with the next 2 minutes, securing advanced airway management within the following 2 minutes, and giving the second adrenaline administration within the next 2 minutes. This protocol allowed for 2 adrenaline administrations during a 10-minute interval in the field, with early administration being practiced.
The prefecture MC councils and local MC councils notify the Fire department about emergency activity protocols, depending on each area. The details regarding adrenaline administration are as follows: “When the initial electrocardiogram rhythm is non-shockable rhythm, administering adrenaline as soon as possible after the EMT contacts patients is suggested. This ‘as soon as’ can be interpreted as administering as quickly as possible in the field. However, considering the environmental factors in the field and transportation times to the hospital, it is possible that transportation will need to be prioritized and therefore in-the-field administration will not be possible. The timing of adrenaline administration can be decided by the local MC council.” [6]. The lack of clarity in this notice leads to differences in adrenaline administration timings, and thus differences in rehabilitation rates.
As discussed in the INTRODUCTION section, previous studies have shown that early adrenaline administration in OHCA patients positively influences ROSC and cerebral function prognoses. To allow for early adrenaline administration, the protocol for its administration in the field should be changed.
First, the protocol needs to be changed from on-line MC to a standard order, which would allow for early adrenaline administration in the field immediately after EMTs arrive at the scene. In 2003, semi-automated external defibrillation was made possible as a standard order, with the aim of ensuring early defibrillation. This change was reported by Iwami et al. [7] as increasing ‘good’ cerebral function prognoses by reducing the time before defibrillation was administered by 3 minutes, compared to defibrillation under on-line MC.
Second, it is essential to manage time efficiently for the giving of adrenaline, before putting patients into the ambulance or within the first 10 minutes of field activity. It is also important to specify the procedure for this protocol, which should be adapted from the suggestions for advanced cardiovascular life support or immediate cardiac life support.
Based on the survey regarding the MC system conducted by the FDMA, local MC councils have changed the timing of adrenaline administration since the 2015 Japan Resuscitation Council guidelines were published. As of August 2017, 113 out of 251 councils (45.0%) have changed their emergency activity protocols, and 183 councils (72.9%) changed these as of August 2018, of which 113 have altered the timing of adrenaline administration [8]. The expected outcome of this was improvement in the number of good ratings for cerebral function prognoses at 1 month postevent.
The national average time for an ambulance to arrive at the scene was 8.6 minutes in 2018, with the shortest average being 8.0±2.3 minutes and the longest being 10.0±2.8 minutes. In order to shorten response times, emergency systems should be reviewed in each area and, if necessary, action taken to improve these. Facing the current situation as response times gets longer, shortening the time periods would not be a simple matter.
However, there are various procedures which could shorten the adrenaline time. Each local MC council, it is suggested, should be reviewed in this respect. IV lines should be secured, and adrenaline administration which is currently under on-line MC should be changed to a standard order. Protocols should be altered to allow administering of adrenaline at the scene before the patient going in the ambulance.
In securing the route for medication administration, intraosseous (IO) lines should be considered. Hubble et al. [9] have demonstrated a higher rate of ROSC when adrenaline is given within 10 minutes of initial contact with EMTs. IO lines can be established 90 seconds faster than IV lines and therefore warrant discussion in Japan.
As response times are getting longer every year, the effects of adrenaline administration will continue to decrease unless adrenaline times shorten. This study proposes use of the prehospital care index to compare objectively the effects of adrenaline on OHCA patients. The timing of administration is reliant on decision-making ability and professional skill, which in turn are contingent on the standard order.
The study had several limitations. First, it was a retrospective study. Second, it was not possible to evaluate cardiopulmonary resuscitation (CPR) that used extracorporeal circulation (E-CPR) in hospital. Third, the quality of bystander CPR and EMT performance was not evaluated.
In conclusion, the timings for administration of adrenaline by paramedics in cases of OHCA in Japan between 2011 and 2014 were examined. The earlier the adrenaline administration was provided, the higher the ratings of good cerebral functioning at 1 month. It is suggested that each local MC council should review this protocol. Adrenaline administration and the security of IV lines should be standardized in terms of practice, with a view to shortening adrenaline administration times, rather than giving adrenaline under on-line MC.
Notes
FUNDING
This study was funded by the Foundation for Ambulance Service Development.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHORS’ CONTRIBUTIONS
Conceptualization: HU; Formal analysis: HTaky, RS; Investigation: HU, HA, HTaka, TK, SS; Methodology: all authors; Project administration: HU, HTan; Supervision: HTan, TH; Writing–original draft: HU, ST; Writing–review & editing: HU, ST.