Time perception in the management of out-of-hospital cardiac arrest
Article information
Abstract
Objective
Time management is a critical aspect in the treatment of out-of-hospital cardiac arrest (OHCA). The American Heart Association guidelines provide specific time frames for critical actions while recommending minimal interruption in chest compression. A variety of factors can alter time perception, but there is limited and conflicting evidence regarding prehospital performance. This study aimed to assess emergency medical services (EMS) personnel’s perception of time and performance during the management of OHCA.
Methods
A retrospective observational study was performed utilizing data obtained from the quality improvement database of a fire-based EMS agency that responds to approximately 10,000 calls for service annually. Data collected over a period of 6 months were reviewed and compared with the actual cardiac monitor data obtained during resuscitation. The primary outcome was the difference between perceived versus actual performance.
Results
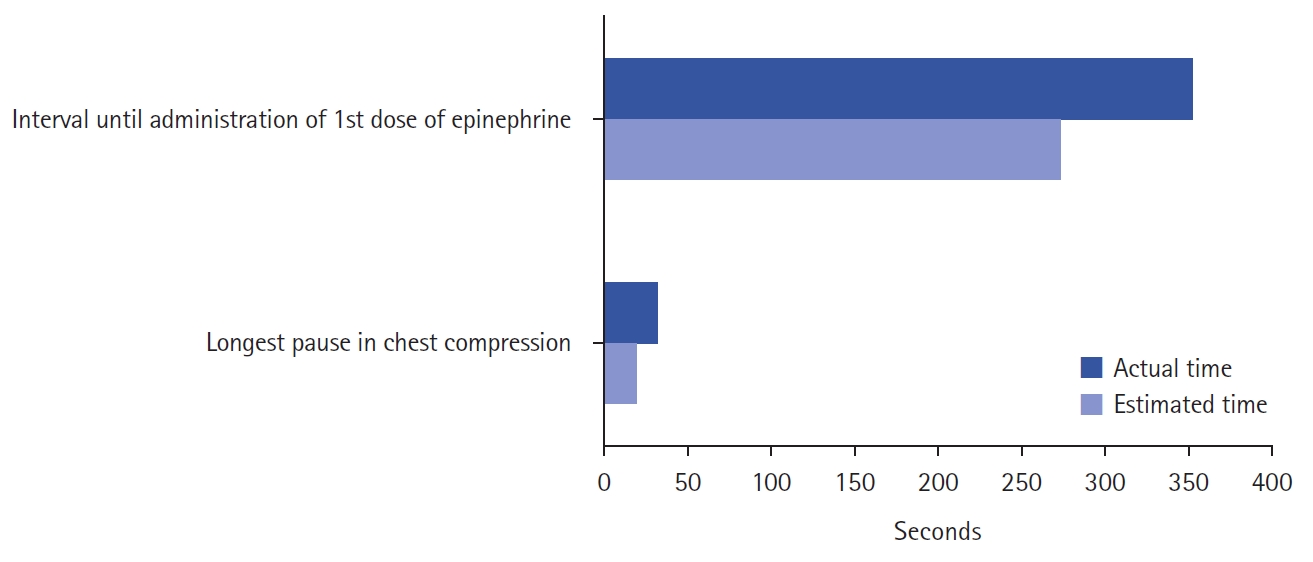
A total of 33 OHCA cases were identified. Twelve cases were excluded due to incomplete data, leaving a final sample size of 21 OHCA cases for analysis. EMS personnel significantly underestimated the length of the longest pause in chest compressions (19.98 seconds vs. 31.99 seconds: 95% confidence interval [CI], 2.62 to 21.43; P=0.013) and significantly underestimated the interval between the initiation of chest compressions and administration of the first dose of epinephrine (274.65 seconds vs. 356.43 seconds: 95% CI, 1.71 to 161.85; P=0.045). No significant difference was found in perceptions of the overall compression fraction (84.4% vs. 87.2%: 95% CI, –5.57 to 3.16; P=0.586).
Conclusion
Our results suggest that EMS personnel underestimate critical time intervals during the treatment of OHCA.
INTRODUCTION
Accurate tracking of elapsed time during attempted resuscitation of cardiac arrest is of great importance, with international guidelines consistently stressing the importance of specific time intervals for certain interventions such as ventilations, and administration of epinephrine [1]. Both the American Heart Association (AHA) and the International Liaison Committee on Resuscitation (ILCOR) recommend high-quality chest compressions with minimal interruption and epinephrine administration as soon as possible for patients with non-shockable rhythms [1,2].
Studies addressing time perception in clinical scenarios are often conducted in an in-hospital-environment and in simulated circumstances [3,4]. The existing literature on time perception in non-simulated scenarios in emergency medical services (EMS) is limited [5]. Previous studies have shown that distortion regarding perceived time on scene in EMS personnel responding to cardiac arrest is common, and passage of time is underestimated in some events and overestimated in others [5-7]. Perception depends on a multitude of factors such as stress, personality, complexity of the situation and may also be affected by emotions and previous experiences. In particularly stressful settings, time is commonly reported as “slowing down” or “standing still,” meaning a time interval may be overestimated [8-11].
However, clinical studies tend to describe an underestimation of time in stressful situations. EMS personnel have been shown to underestimate time spent on scene [5]. Similarly, Kuhlenschmidt et al. [12] reviewed video of non-simulated trauma resuscitations and concluded physicians underestimate elapsed time by up to 28%, such that if the resuscitation lasted 20 minutes, the clinicians’ perception was that only 14.4 minutes of elapsed time. Trevisanuto et al. [3] found similar underestimation in perceived time for the initiation of key interventions in simulated neonatal resuscitations.
This study aims to assess the perception of time and performance of first responders during the management of out-of-hospital cardiac arrest (OHCA), a notoriously high-stress, time-critical event.
METHODS
In this retrospective observational study, self-reported perception of time and performance in three key metrics associated with management of OHCA were compared to the actual clinical data. Data were collected within a moderately sized, suburban, fire-based EMS system responding to approximately 10,000 9-1-1 medical calls for service annually. All responding ambulances are licensed for advanced life support and are staffed by at least one paramedic or EMT-Intermediate.
A convenience sample of post-arrest surveys, completed by EMS personnel immediately after attempted resuscitation of a confirmed cardiac arrest, was reviewed. The surveys obtained data on the responder role during the resuscitation and several key metrics including the estimated time elapsed from the start of resuscitation until the first dose of epinephrine, the estimated duration of the longest pause in chest compressions and the estimated overall compression fraction. Incident numbers were used to match survey responses to data obtained from the Zoll X-Series cardiac monitor used during the corresponding resuscitation. Utilizing the cardiac monitor data, available through the Zoll Online platform, pause length and compression fraction were determined. Utilizing the ImageTrend electronic patient care record, time of epinephrine administration could be determined and crosschecked with manual timestamps, made by the treating EMS personnel on the cardiac monitor.
A total of 33 OHCA were identified during a 6-month period with 140 corresponding surveys. After exclusion of cases with incomplete survey or monitor data, a total of 21 OHCA cases and 81 survey responses remained for analysis. The primary outcome of the study was the difference between the perceived time interval and the actual time interval. Statistical analysis was performed using the online software GraphPad. Time interval differences were compared using t-tests with a P-value of less than 0.05 considered to be statistically significant.
This study was reviewed and approved as exempt by an institutional review board.
RESULTS
Comparison of post-arrest survey responses and monitor data showed first responders’ perception of the longest pause in chest compressions was significantly shorter than the actual longest pause (19.98 seconds vs. 31.99 seconds: 95% confidence interval [CI], 2.62 to 21.43; P=0.013). The interval between initiation of chest compressions until the administration of the first dose of epinephrine was similarly underestimated (274.65 seconds vs. 356.43 seconds: 95% CI, 1.71 to 161.85, P=0.045). No difference was found between the responders’ perception of overall compression fraction and actual values (84.4% vs. 87.2%: 95% CI, –5.57 to 3.16; P=0.586). Subgroup analysis of code leaders showed an underestimation of length of longest pause in chest compression (18.42 seconds vs. 31.99 seconds: 95%, 4.97 to 22.19; P=0.003), however, they otherwise accurately perceived the interval between the initiation of chest compressions and administration of the first dose of epinephrine and the overall compression fraction (Table 1, Fig. 1).
DISCUSSION
Our results suggest that first responders underestimate critical time intervals associated with managing OHCA. While this study was not designed to assess patient-centered impacts of time perception, prolonged interruptions in chest compressions in OHCA are associated with decreased coronary and cerebral perfusion and therefore lower likelihood of return of spontaneous circulation and survival [13].
EMS personnel also significantly underestimated the interval to administration of the first dose of epinephrine, meaning that more time passed until they administered the epinephrine than they perceived. Although a source of great controversy and ongoing research, recent findings suggest that early epinephrine administration may be associated with better survival outcomes in adults with OHCA [14]. The most recent AHA and ILCOR guidelines reaffirm early epinephrine administration for non-shockable cardiac arrest [1,2].
Subgroup analysis showed that code leaders also tend to underestimate the total length of the longest pause in chest compression, but otherwise accurately perceived their overall performance. Whether this slightly better estimation of time and performance in code leaders can be explained by higher levels of training and/or experience, or their specific role in the scenario is unclear. According to several studies, the participant’s role in the scenario has no effect on time perception and some may simply have a better innate sense of time perception than others [3,12].
Our data suggest a tendency to underestimate time in a high-stress clinical scenario. Cognitive psychology studies involving adult volunteers have shown that participants tend to overestimate the perceived time duration when exposed to high arousal or traumatic conditions or to negative emotional states like fear or negative stress [8,10]. However, like other clinically based studies of time perception, our results show underestimation of time interval. A reason for this underestimation of time might be that EMS personnel feel excitement and satisfaction while performing their tasks during an attempted resuscitation, rather than fear or negative stress [15].
Some limitations must be considered when interpreting these results. Small sample size and wide CIs suggest the need for larger studies, preferably with the addition of patient-centered outcomes data. Additionally, although surveys were generally collected immediately following the case, on occasion it can be assumed the crew would be sent to another call or have some other delay in completing the survey leading to recall bias. Although asked to complete the surveys individually and without accessing monitor data or other sources of time stamped data, and there would be no plausible benefit to the individual, this could have occurred. Lastly, the volume of missing data raises the question of responder bias and device accuracy. One particular issue encountered was the inability of the cardiac monitor to detect manual or mechanical chest compressions if not performed directly over the accelerometer. Inadvertent displacement of the compression accelerometer resulted in a significant loss of data, with no compressions recorded and appearing as extremely prolonged pauses.
In conclusion, our results suggest that first responders underestimate critical time intervals associated with managing OHCA. The collected data showed EMS personnel significantly underestimated the length of the longest pause in chest compressions and significantly underestimated the interval between the initiation of chest compressions and administration of the first dose of epinephrine. The effect on patient-centered outcomes associated with these aberrations in time perception is unknown and represents an opportunity for further study.
Notes
FUNDING
None.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHORS’ CONTRIBUTIONS
Conceptualization: AL, HA; Data curation: AL, HA; Formal analysis: AL, HA; Methodology: all authors; Supervision: AL; Validation: GB, AL; Writing–original draft: GB; Writing–review & editing: all authors.
ACKNOWLEDGMENTS
We thank the emergency medical service personnel from the James City County Fire Department for their eager participation in this study.