|
 |
- Search
| J EMS Med > Volume 2(3); 2023 > Article |
|
Abstract
Objective
This study assessed the feasibility, acceptability, and subsequent healthcare utilization following diversion of low-acuity 911 calls to hospital-based telemedicine.
Methods
Eligible 911 calls were transferred to hospital-based call centers for further triage and evaluation. An ambulance was dispatched for calls deemed inappropriate for telemedicine. Otherwise, further evaluation and treatment were provided by a nurse practitioner/physician assistant, or a telehealth visit was initiated. Follow-up calls were attempted on all patients within 48 hours.
Results
In total, 454 calls were diverted to the triage line. Approximately 18.5% of the calls were related to coronavirus disease 2019 (COVID-19). An ambulance was dispatched for 60.4% of the completed calls. The proportion of calls resulting in ambulance response increased as the pandemic improved. Among appropriate transfers, 31.7% received additional triage and did not require an ambulance. Seventy-seven patients (17.0%) received medical advice over the phone, but only 39 (8.6%) were able to complete a telemedicine evaluation. Among the 315 attempted follow-ups, 142 patients (45.1%) were contacted. A small proportion of patients (8.6%) called 911 again after triage. Thirty-seven patients were admitted to the hospital after the initial call, with one patient in intensive care unit.
Conclusion
Our institution successfully diverted selected 911 calls to hospital-based telemedicine, resulting in fewer ambulance dispatches and more appropriate allocation of emergency medical services resources. However, many callers sought subsequent care after diversion with some requiring hospitalization, and patient acceptance of diversion decreased as pandemic conditions improved. More specific initial screening algorithms, public education campaigns, and streamlined telemedicine workflows could significantly increase the effectiveness of similar programs.
The first and second waves of the coronavirus disease 2019 (COVIDŌĆÉ19) pandemic affected the New York City (NYC) metropolitan area during the spring and fall of 2020 resulting in the highest 911 call volume and ambulance dispatches in the history of NYC emergency medical services (EMS) [1]. NYC experienced unprecedented demand for healthcare services during the first surge with 2,000 to 6,000 new cases diagnosed per day between March and May of 2020 [2]. These increases in volume were also accompanied by increased acuity: rates of respiratory failure were 10 times higher than prior estimates (COVID-19 intubation rate: 33.1, standard intubation rates in all U.S hospitals being estimated between 3% and 5%) [3,4].
NYCŌĆÖs EMS system is the busiest in the United States and averages 4,000 calls per day serving a population of 8.4 million. The high-volume system received an additional 1,128 911 calls per day compared with the same period in 2019. As a result, the average ambulance response time was 36 minutes slower than the previous year. Additional units were supplied by local mutual aid and outŌĆÉofŌĆÉstate ambulance providers coordinated through the Federal Emergency Management Agency. However, demand for ambulance responses continued to increase with increasing case counts, and outpaced this supplemental capacity [1]. To better triage increasingly limited resources, several area hospitals collaborated with the New York City Fire Department (FDNY), which oversees the NYC 911 system to transfer lowŌĆÉacuity patients to hospital-based telemedicine for further triage and evaluation without an immediate ambulance response.
Prior to this initiative, telehealth had not been used in the NYC EMS system, however other large municipalities have successfully utilized telemedicine services in the prehospital setting for advanced triage of low acuity complaints [5]. Given these successes and building upon ongoing collaborative work to implement the Centers for Medicare & Medicaid Innovations Emergency Triage, Treat and Transport (ET3) in the NYC region, our academic health system, along with other local health systems and FDNY developed triage criteria, workflows and reciprocal legal agreements to divert appropriate 911 callers to hospital-based telemedicine for further triage, treatment and referral as appropriate. Unlike ET3 and other EMS-based telemedicine services, no in-person evaluation would take place via an ambulance dispatch/EMS provider.
To our knowledge EMS calls have never been transferred to telemedicine without an in-person evaluation [6]. Data from trauma and stroke patients along with the medico-legal climate have driven EMS culture, protocols and innovation with a focus on prompt prehospital assessment, stabilization and emergency department (ED) transfer [6-8]. Nationwide ET3 implementation will provide the opportunity to utilize prehospital providers and infrastructure to a fuller extent. However, limited data exists as to whether patients with lower acuity complaints can be safely treated via telehealth without an EMS or provider face-to-face evaluation. Less is known about patient acceptance of programs diverting 911 callers to alternative workflows that do not involve in-person evaluation or ambulance transport under varying conditions.
The goal of this study was to assess feasibility and patient outcomes after diversion of 911 callers to hospital-based telemedicine programs during different phases of the COVID-19 pandemic in NYC. Specifically, we wanted to determine the number and characteristics of diverted callers successfully transferred to a telemedicine provider and assess subsequent healthcare utilization including EMS utilization and hospital admissions as an estimate of patient safety and acceptance. We hypothesized that caller acceptance of diversion to telemedicine would decrease as COVID-19 prevalence in NYC decreased.
911 Calls received from all five boroughs in NYC via FDNY dispatch from April 3, 2020, to October 2, 2020, were screened for specific inclusion and exclusion criteria by trained emergency medical dispatchers (EMD) using a computerized algorithm (Fig. 1). Patients aged 5 to 59 were eligible given the patient was the caller (or an adult parent calling for a minor present) and the patient was located in a safe location where a telemedicine encounter could be performed (i.e., patient is not on the street). Inclusion criteria for transfer were based on predetermined call types determined by the EMD. All FC (fever and cough; which could be added to any call type concerning for possible COVID-19 infection) were eligible. Respiratory complaints (RESPIR) were eligible if designated FC and did not meet any of the following exclusion criteria: can speak in full sentences, no associated chest pain, no cardiac, asthma, or chronic obstructive pulmonary disease history, and has never been intubated in the past). Minor medical complaints not fitting into other call type categories were eligible, typically designated by SICK (including, but not limited to sore/abscess/boil, chills, dizziness/vertigo, fever, diarrhea, constipation, nausea, vomiting, headache, other non-chest pain, rash, sickle cell crisis, or swelling) or SICMIN (including, but not limited to earache, malaise, genital problem, medication refill, respiratory symptoms including cough, congestion, or cold symptoms, toothache, or urinary problems) call types.
Eligible calls were transferred by the EMD to a hospital-based hotline. Callers were asked ŌĆ£what hospital do you normally go to for your healthcare?ŌĆØ and transfers were based on the health system affiliated with that hospital; for patients without an established healthcare provider, callers were randomly assigned to a telemedicine service. Callers were then connected to a team of nine staff nurse practitioners (NP) or physician assistants (PA) via telephone for further remote triage (RT). This line was staffed when call volumes were highest: 12 hours per day, 5 days per week to allow for provision of medical advice or transfer to telemedicine provider as appropriate. Triage NP/PAs were able to dispatch ambulances using the FDNY incident number for calls deemed not appropriate for telemedicine after further RT. Triage NP/PAs could provide medical advice, prescribe medications, schedule follow-up appointments and/or facilitate initiation of a video visit with an emergency physician staffing our institutional virtual urgent care service line. Workflows were provided for NP/PAs to assist callers with downloading and scheduling virtual urgent care appointments. Follow-up calls were attempted on all patients within 48 hours of initial 911 call by a dedicated registered nurse with care management certification (RN) during the first 3 months of the program to assess patient outcomes, provide additional medical advice or clinical navigation, and collect information on subsequent healthcare utilization.
Data on age, caller location, medical comorbidities, history of present illness, and call outcomes were entered directly into the study database using a secure web-based survey form during the initial call by NP/PAs performing RT. Follow-up calls attempted by the RN used a structured telephone script and data collection form to evaluate callers the persistence of symptoms, the type and timing of additional medical care sought including repeat 911 activation, ambulatory clinic visits, ED visits, and hospital admissions including intensive care unit admissions. Data were reviewed by three clinicians not involved in the initial call-taking process (WH, ML, and BD) and an Emergency Severity Index (ESI) score was assigned by each provider based on chart review, agreement between assigned ESI levels was assessed, and discrepancies were averaged. As RT did not include evaluation of vital signs, ESI was assigned based on the presence of immediate threat to life or limb requiring emergency intervention (ESI level 1), high risk criteria such as altered mental status, severe distress or pain (ESI level 2), and the number of anticipated resources required such as laboratory test, radiology or intravenous medication (many, one, none indicated ESI level 3, 4 or 5 respectively). Since abnormal vital signs are typically used to up-triage ESI 3 to ESI 2, we assumed any patients reporting significant respiratory or cardiac symptoms would be triaged to ESI2. Study data were collected and managed using a secure interface termed: REDCap (Research Electronic Data Capture). REDCap is a secure, web-based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for data integration and interoperability with external sources [9,10]
Caller demographics reported medical comorbidities, caller origination, chief complaint organ system, and disposition were computed as frequencies. Reasons for ambulance dispatch after remote are reported along with type and frequency of follow-up care after initial call. Weekly call volumes were compared to COVID case counts using data publicly available from the New York City Department of Health [2]. Chi-square and analysis of variance tests to examine differences in characteristics between patients in early and late 2020, coinciding with dropping COVID-19 case numbers during the summer and fall of 2020 [2]. Differences in the reason for ambulance dispatch between early and late 2020 emergency calls were examined by odds ratios (OR) obtained from multivariable logistic regression models. Crude differences are reported in addition to results adjusted for patient demographics (age, sex, and borough). Comparisons between these time periods for ESI were reported as mean differences from t-tests. The inter-rater reliability of three individual ESI ratings was evaluated using LightŌĆÖs kappa [11,12]. An alpha of 0.05 was used for hypothesis testing and all statistical analyses were performed using R v4.1.112. This study was approved by the Weill Cornell Medical College Institutional Review Board (IRB) (No. 21-09023955). Informed consent was waived by the IRB.
Four hundred and fifty-seven calls were transferred to our telemedicine service from April 3, 2020, to October 2, 2020 (Fig. 2). Call volume varied by week with an average of 3.8 calls per day (median, 4; range, 0-14). The highest daily number of diverted calls (n=14) were transferred on 4 of 27; multiple dates had no calls diverted to telemedicine. Three calls (0.7%) had no interaction between provider and patient and were removed from the analysis. As shown in Table 1, calls originated throughout all boroughs across NYC, however the majority were from the Bronx (16.5%), Brooklyn (14.5%), and Manhattan (13.2%); fewer calls were received from Queens (9.7%) and a small proportion (1.5%) were from Staten Island.
The average age of the 454 included callers was 43.3 years (interquartile range, 31.0ŌĆō54.1 years). Female callers made up slightly less than half (46.9%) and 3.1% were pediatric (less than 18 years old). Most patients (85.5%) had at least one medical problem: 22.9% had hypertension, 16.1% had diabetes, and 5.3% had heart disease, 7.7% were immunosuppressed and 11.7% and 4.8% had lung and kidney disease, respectively. Comparing demographics between the early phase of the initial COVID-19 pandemic in NYC and the later phase, callers during periods of lower COVID case counts were less likely to have significant comorbidities, specifically hypertension, diabetes or be immunosuppressed.
Table 2 compares presenting complaints, ESI triage level and call outcomes between the initial and late phases of the first COVID-19 wave in NYC. Overall, 18.5% of calls were determined to be related to COVID after RT with a statistically significant decrease in COVID-19-related calls (26.0% to 10.8%, P=0.004) between early months of the initial pandemic wave and the latter. Respiratory-related calls also dropped significantly between the two time periods (P=0.008). There were 8.6% more musculoskeletal-related complaints during the second period relative to the first while all other complaint categories remained static: 18.3% were related to the gastrointestinal system and 17.6% related to the musculoskeletal system. Neurologic (13%), respiratory (12.8%), and cardiovascular (10.4%) were the next most common complaints followed by ear/nose/throat, genitourinary, and dermatological, which were each less than 10%.
ESI was assigned retrospectively. One patient had an ESI of 1 and 4.4% were assigned ESI of 2. Most patients (56.8%) were assigned ESI 3, followed by ESI 4 (28.9%). Few patients (4.8%) were assigned an ESI level of 5. Agreement between reviewers was good: all three reviewers agreed in 79.6% of cases and 87.0% of remaining disagreements differed by only one ESI point. There was weak/fair inter-rater reliability in individual ESI estimates (k=0.33, P<0.001).
Of 454 calls placed to 911, 200 (44.1%) were determined not to be appropriate for telemedicine at the time of transfer to the hospital-based telemedicine program. An additional 74 callers (16.3%) required an ambulance response after completion of RT by the NP or PA. In total, 274 (60.4%) resulted in an ambulance response despite being diverted to telemedicine. A minority of callers 36 (7.9%) hung up during RT, however, approximately twice as many callers hung-up during the height of the pandemic (10%) versus the latter period once case counts were decreasing (4.9%, P=0.042).
Of the 180 callers completing remote triage, 77 (17.0%) had their complaints addressed via the RT provider and did not require an ambulance response nor complete a telemedicine visit. 39 (8.6%) patients eligible for a virtual urgent care visit successfully completed a telemedicine encounter: although uncommon, telemedicine visits occurred more frequently during the height of the pandemic (14.3% vs. 2.7%, P<0.001). Conversely, ED referrals via personal transport (5.1%) were more common during the end of the first COVID wave in NYC (8.5% vs. 1.7%, P<0.001).
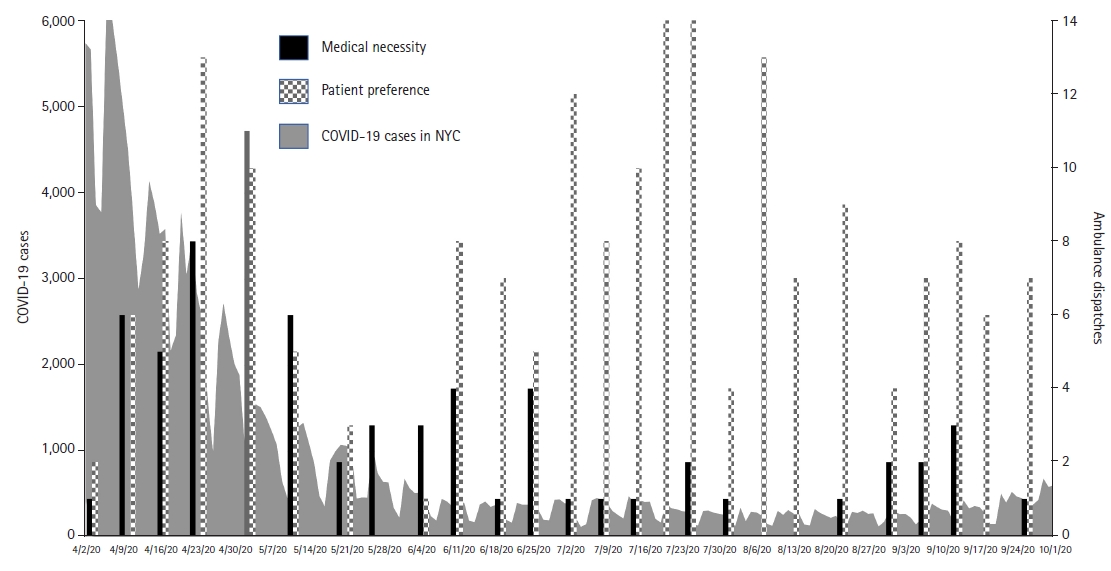
Ambulance dispatches after transfer to hospital-based telemedicine services were categorized as either due to medical necessity or patient preference: 188 (68.6%) were due to patient preference while 69 (25.2%) were due to medical necessity. During the initial pandemic wave, 129 patients required an ambulance with 49.6% due to patient preference and 41.1% due to medical necessity (Fig. 3). From June until October, when COVID-19 case counts were decreasing across the city, 145 patients required an ambulance with the majority (85.5%) due to patient preference (OR, 6.8; 95% confidence interval, 3.65ŌĆō13.38). A higher likelihood of ambulance dispatch due to patient preference was observed after adjusting for caller characteristics including age, sex, and borough during the second study period (OR, 6.2; 95% confidence interval, 2.41ŌĆō18.27).
Follow-up phone calls were performed during the first three months after launch of the intervention. Among 315 (69.4%) attempted calls, we successfully followed up with 31.3% of patients. Nearly two-thirds of patients received medical care in an ED or urgent care after their initial 911 call. Approximately one-quarter (26.1%) were admitted, with one patient requiring intensive care unit level care (this patient was deemed not suitable for telemedicine after RT). Twenty (14.1%) patients for whom an ambulance was dispatched were evaluated by EMS in the field, but ultimately were not transported to the hospital. A small proportion of patients (7.8%) diverted to telemedicine called 911 back immediately, while 12 (8.5%) patients went to the ED on their own. Of the group of patients who called 911 immediately or went to the ED on their own, 18 (78.2%) were admitted. Nine patients (6.3%) contacted their primary care provider and 11 of the patients who did not seek medical care after the call indicated they completed a telemedicine visit.
There are a few notable limitations of our study. All caller information was obtained by self-report during the RT evaluation, which many callers did not complete. Estimates of patient acuity were limited by the lack of available vital signs typically used in the determination of ESI level. However, multiple reviewers were used to determine ESI and the primary interest of our study was to compare ESI during the early and later phases of the pandemic such that any limitations should be consistent across the two time periods.
We were not able to view patient health records or systematically assess outcomes after the diversion to RT and/or telemedicine. Our follow-up with patients was also incomplete, with less than one-third successfully contacted for follow-up. Furthermore, this cohort is limited to callers diverted to our hospital-based telemedicine program and call type and outcomes may have differed at different institutions. However, this is the first study to our knowledge to attempt to contact patients after 911 diversion to telemedicine. Finally, our program was implemented during the height of the COVID-19 pandemic, and while our study period extends to the tail-end of the initial wave, this context significantly limits the generalizability of our study results.
We successfully participated in an NYC-wide pilot to divert selected 911 calls to hospital-based telemedicine, reducing ambulance dispatches by 40% during the height of the first wave of the COVID-19 pandemic. The importance of this is not to be understated, given current nationwide staffing shortages of EMS personnel [13] along with rising costs of providing ambulance services [14]. Notably, 274 ambulances were dispatched from the 454 calls deemed eligible for telemedicine after computerized triage and EMD evaluation. Some of these patients were incorrectly triaged and upon initial transfer ambulance dispatch was immediately deemed necessary. Current studies have involved utilizing more sophisticated screening algorithms to identify patients suitable for telemedicine [15]. Utilizing this may improve the ratio of ambulance dispatches to those diverted to telemedicine. Conversely other studies have suggested the additional layer of triage, such as the NP/PA utilized in our model is necessary and should not be omitted [16].
Although inappropriate diversion was common in our program, many ambulances were ultimately dispatched by patient request despite being offered alternatives. This was particularly true as the pandemic wore on, and patients seemed less amenable to referral to telemedicine in lieu of an ambulance response. This suggests that acceptance may be related to the perceived risk of going to the hospital at the height of the pandemic. Many of these patients likely could have been safely transported to the ED or other health care facility without an ambulance or evaluated by telemedicine. Prior data suggests that nearly 60.0% of all ambulance-transported patients were deemed non-emergent with 74% discharged within the same day of 911 request [17].
Public education campaigns to inform 911 caller expectations and qualitative studies to better understand patient perceptions of 911-to-telemedicine diversion programs may improve the success rate of transfer and decrease the unnecessary care-seeking behavior observed in our study after diversion. While patient expectations and acceptance need to be addressed, additional barriers to telemedicine have been cited including lack of computer literacy, low socioeconomic status, and age [18]. The limitations of these factors are demonstrated in our results, 77 patients only received medical advice over the phone from the RT provider and did not elect to pursue a telemedicine encounter. The extra technology and complexity (and associated cost) of obtaining a telehealth evaluation as compared to a phone call likely played a role in this.
Limitations regarding patient preference of care locations can likely be aided with public education, given that only 58% of patients agreed with EMS transport to alternative destinations [19]. which falls in line with our numerous ambulance dispatches for patient preferences and 7.8% of patients calling 911 immediately after telemedicine for ambulance dispatch. Public health has had success with this in the past in the prehospital arena with messaging on cerebral vascular accident signs and symptoms [20] and could be replicated in a similar manner to improve perception of telemedicine and its role in EMS.
Given some of our callersŌĆÖ resistance to telemedical evaluation, a hybrid model could provide in-person evaluation from EMS along with telemedical evaluations from providers could reduce EMS and ED burden [5]. Others have implemented similar models with notable cost savings [21]. The Emergency Treat, Triage, and Transport model (ET3), which was implemented in 2021, and incentivizes ambulance providers to offer alternative destination transport and treatment-in-place via telemedicine to Medicare patients calling 911 [22] will likely encounter similar mis-triage and patient acceptance limitations. The results of our study may help inform ongoing quality improvement processes for ET3 participants and partners.
Fig.┬Ā1.
Workflow for diversion of low acuity 911 calls to hospital-based telemedicine service. Patients with suspected coronavirus disease 2019 (COVID-19) or minor complaint call type determined by computerized triage algorithm and emergency medical dispatcher meeting eligibility criteria were transferred to a hotline staffed by a nurse practitioner (NP) or physician assistant (PA) for further remote triage and clinical navigation. SIC, low acuity call type; FAQ, frequently asked questions (referred to 311 COVID hotline); PMD, primary care provider; ED, emergency department.
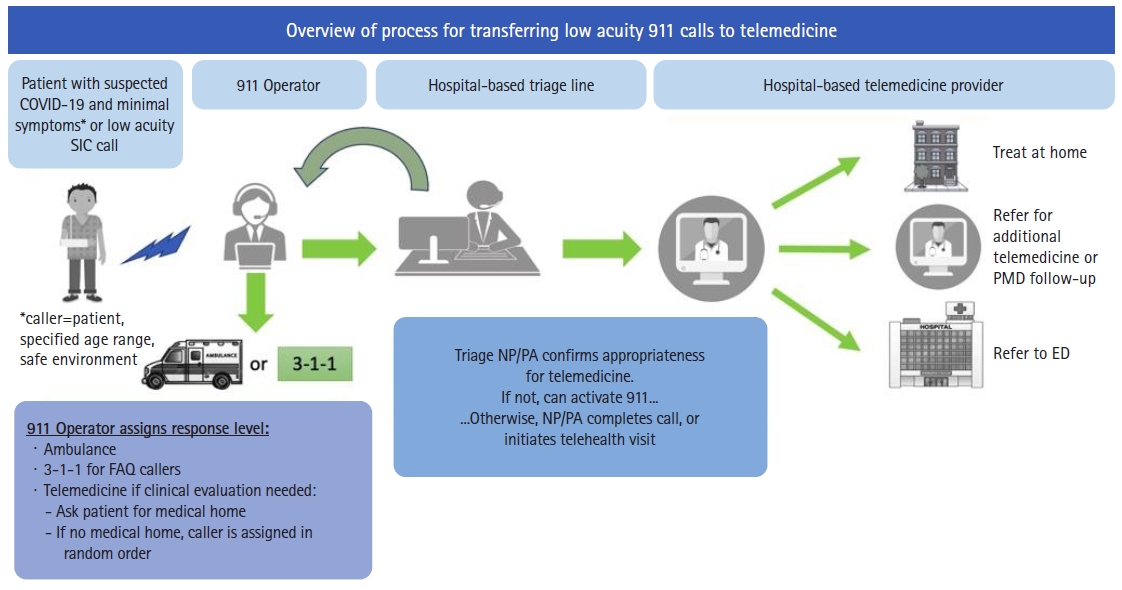
Fig.┬Ā2.
Flowchart of 911 callers diverted to hospital-based remote triage (RT) and call outcomes. Among diverted callers, 200 (44%) did not undergo RT because triage was deemed inappropriate upon initiation of RT due to medical necessity or patient request. Outcomes are shown for the 254 callers completing sufficient RT to determine disposition. ED, emergency department.
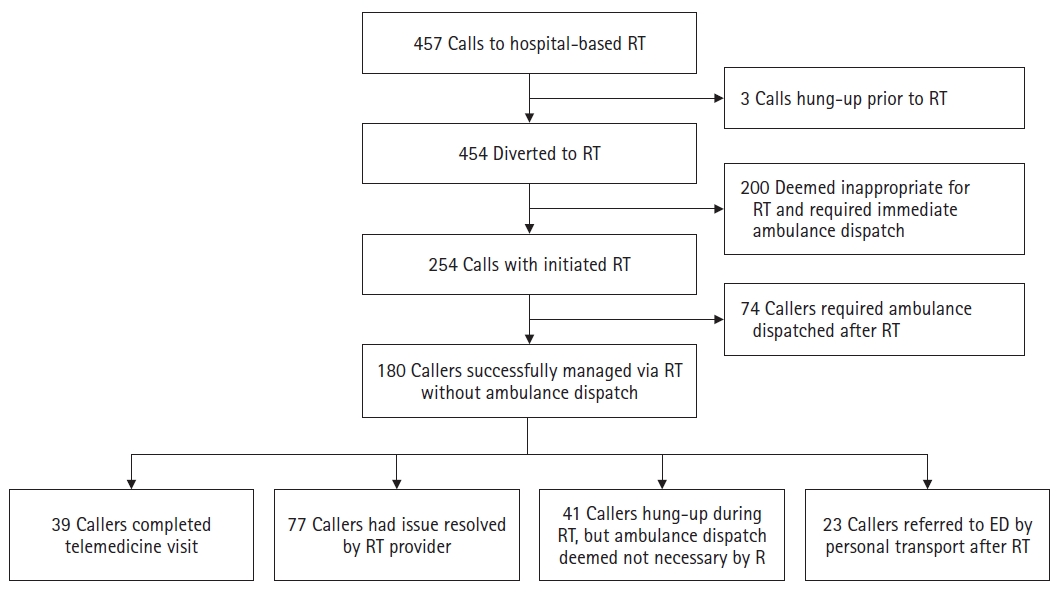
Fig.┬Ā3.
Comparison of coronavirus disease 2019 (COVID-19) case counts and reasons for ambulance dispatch after remote triage following 911 diversion to telemedicine by week from April to October 2020. Gray line corresponds to the number of new COVID-19 cases reported (left y-axis) in New York City (NYC) with an overlying black/histogram representing the relative percent of ambulance dispatches due to medical necessity versus patient preference (right y-axis) by week. A higher proportion of ambulance dispatches were secondary to patient preference rather than medical necessity as COVID-19 positivity rates decreased.
Table┬Ā1.
Characteristics of 911 callers diverted to hospital-based telemedicine
a)For some callers not enough information was provided to ascertain Sex, Medical History, and/or caller location; b)Myocardial infarction or heart failure; c)HIV (human immunodeficiency virus), steroids, transplant, or on chemotherapy; d)P-values were not computed for these values due to the low sample size of pregnant, pediatric, and Staten Island.
Table┬Ā2.
Characteristics, ESI level, and call outcomes among 911 calls diverted to telemedicine
Values are presented as number (%).
ESI, Emergency Severity Index; COVID-19, coronavirus disease 2019; RT, remote triage; No evaluation, caller was unable to be evaluated for medical or technical reasons; ED, emergency department.
a)Due to low volume of callers, results from September to October are not represented in this table.
REFERENCES
1. Prezant DJ, Lancet EA, Zeig-Owens R, et al. System impacts of the COVID-19 pandemic on New York CityŌĆÖs emergency medical services. J Am Coll Emerg Physicians Open 2020;1:1205ŌĆō13.




2. New York City Department of Health and Mental Hygiene. COVIDŌĆÉ19: Data and Death Rate 2020 [Internet]. New York, NY: New York City Department of Health and Mental Hygiene; 2020 [cited 2022 Sep 30]. Available from: https://www.nyc.gov/site/doh/covid/covid-19-data-totals.page.
3. Goyal P, Choi JJ, Pinheiro LC, et al. Clinical characteristics of COVID-19 in New York City. N Engl J Med 2020;382:2372ŌĆō4.



4. Pfuntner A, Wier LM, Stocks C. Most Frequent Conditions in U.S. Hospitals, 2011. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville, MD: Agency for Healthcare Research and Quality (US); 2006 [cited 2022 Sep 30]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK169248/.
5. Langabeer JR 2nd, Gonzalez M, Alqusairi D, et al. Telehealth-enabled emergency medical services program reduces ambulance transport to urban emergency departments. West J Emerg Med 2016;17:713ŌĆō20.



6. Bergrath S, Brokmann JC, Beckers S, Felzen M, Czaplik M, Rossaint R. Implementation of a full-scale prehospital telemedicine system: evaluation of the process and systemic effects in a pre-post intervention study. BMJ Open 2021;11:e041942.



7. Ornato JP, Craren EJ, Nelson NM, Kimball KF. Impact of improved emergency medical services and emergency trauma care on the reduction in mortality from trauma. J Trauma 1985;25:575ŌĆō9.


8. Georgakakos PK, Swanson MB, Ahmed A, Mohr NM. Rural stroke patients have higher mortality: an improvement opportunity for rural emergency medical services systems. J Rural Health 2022;38:217ŌĆō27.




9. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377ŌĆō81.



10. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208.



12. Light RJ. Measures of response agreement for qualitative data: some generalizations and alternatives. Psychol Bull 1971;76:365ŌĆō77.

13. Hill R. EMS Company hopes nationwide staffing shortage for themselves & others with more graduates as pandemic restrictions ease. GoodDayCW31. May 27, 2021 [cited 2022 Sep 30]. Available from: https://www.cbsnews.com/gooddaysacramento/news/ems-company-hopes-nationwide-staffing-shortage-for-themselves-others-with-more-graduates-as-pandemic-restrictions-ease/.
14. Morabito C. Why taking an ambulance is so expensive in the United States. CNBC. Jul 10, 2020 [cited 2022 Sep 30]. Available from: https://www.cnbc.com/2020/07/10/why-taking-an-ambulance-is-so-expensive-in-the-united-states.html.
15. Kang DY, Cho KJ, Kwon O, et al. Artificial intelligence algorithm to predict the need for critical care in prehospital emergency medical services. Scand J Trauma Resusc Emerg Med 2020;28:17.




16. Scott G, Clawson J, Fivaz MC, et al. Using on-scene EMS respondersŌĆÖ assessment and electronic patient care records to evaluate the suitability of EMD-triaged, low-acuity calls for secondary nurse triage in 911 centers. Prehosp Disaster Med 2016;31:46ŌĆō57.


17. Jones CM, Wasserman EB, Li T, Shah MN. Acceptability of alternatives to traditional emergency care: patient characteristics, alternate transport modes, and alternate destinations. Prehosp Emerg Care 2015;19:516ŌĆō23.


18. Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare 2018;24:4ŌĆō12.




19. Munjal KG, Shastry S, Loo GT, et al. Patient perspectives on EMS alternate destination models. Prehosp Emerg Care 2016;20:705ŌĆō11.


20. Mellon L, Doyle F, Rohde D, Williams D, Hickey A. Stroke warning campaigns: delivering better patient outcomes? A systematic review. Patient Relat Outcome Meas 2015;6:61ŌĆō73.