|
 |
- Search
| J EMS Med > Volume 2(2); 2023 > Article |
|
Abstract
Objective
Methods
Results
ACKNOWLEDGEMENTS
Funding
This study was supported by the Graduate school of EMS, Kokushikan University in Japan, Navamindradhiraj University for supporting the scholarship, and Mr. Anurut Somton from the National Institute of Emergency Medicine for the original data support.
Authors’ contributions
Conceptualization: DT; Data curation: DT; Formal analysis: DT, HTak; Investigation: DT, HTak; Methodology: DT, HTak; Project administration: DT; Resources: DT, HTak; Software: HTak; Supervision: DT; Validation: all authors; Visualization: DT; Writing–original draft: DT; Writing–review & editing: DT, HTan.
Fig. 2.
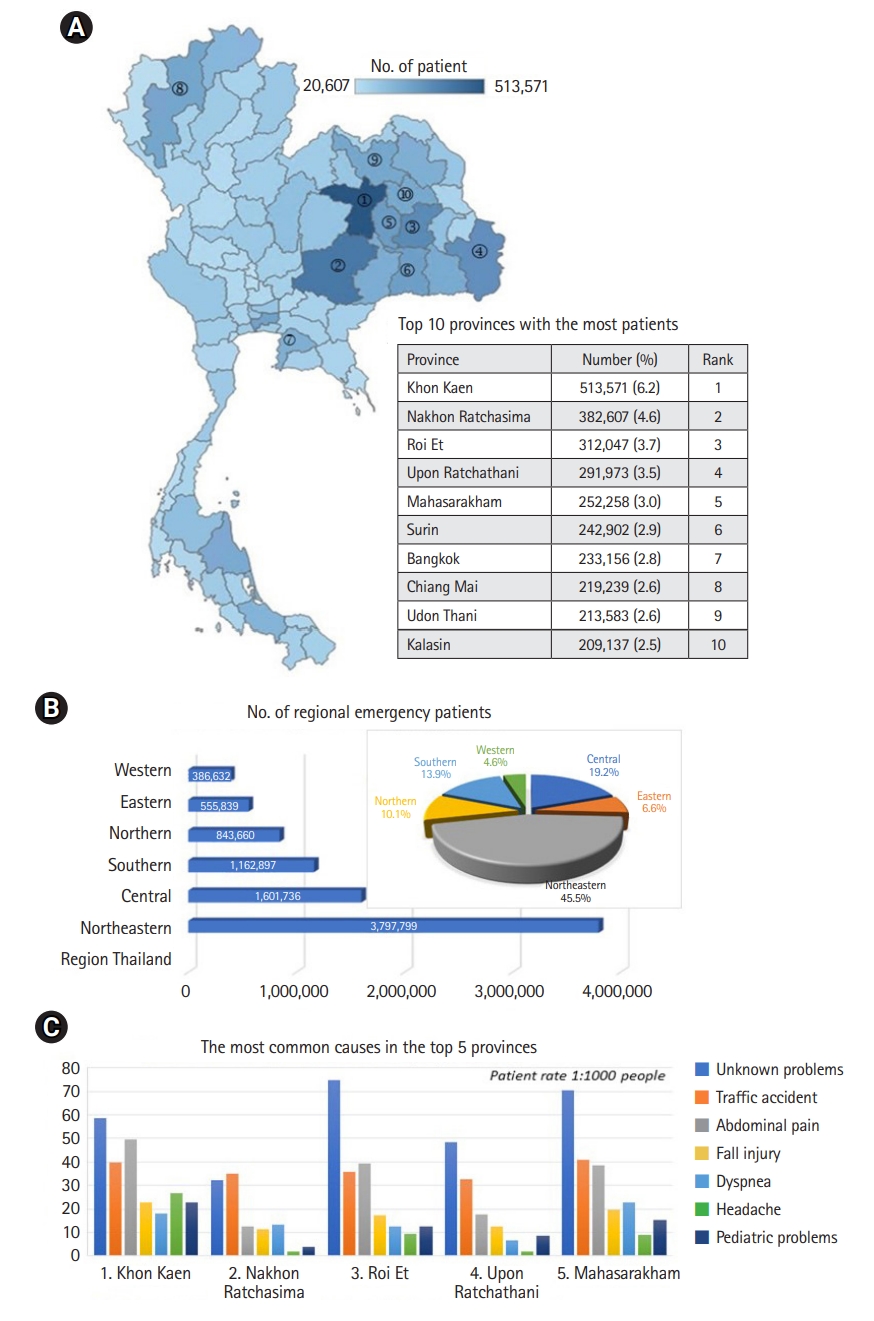
Fig. 3.
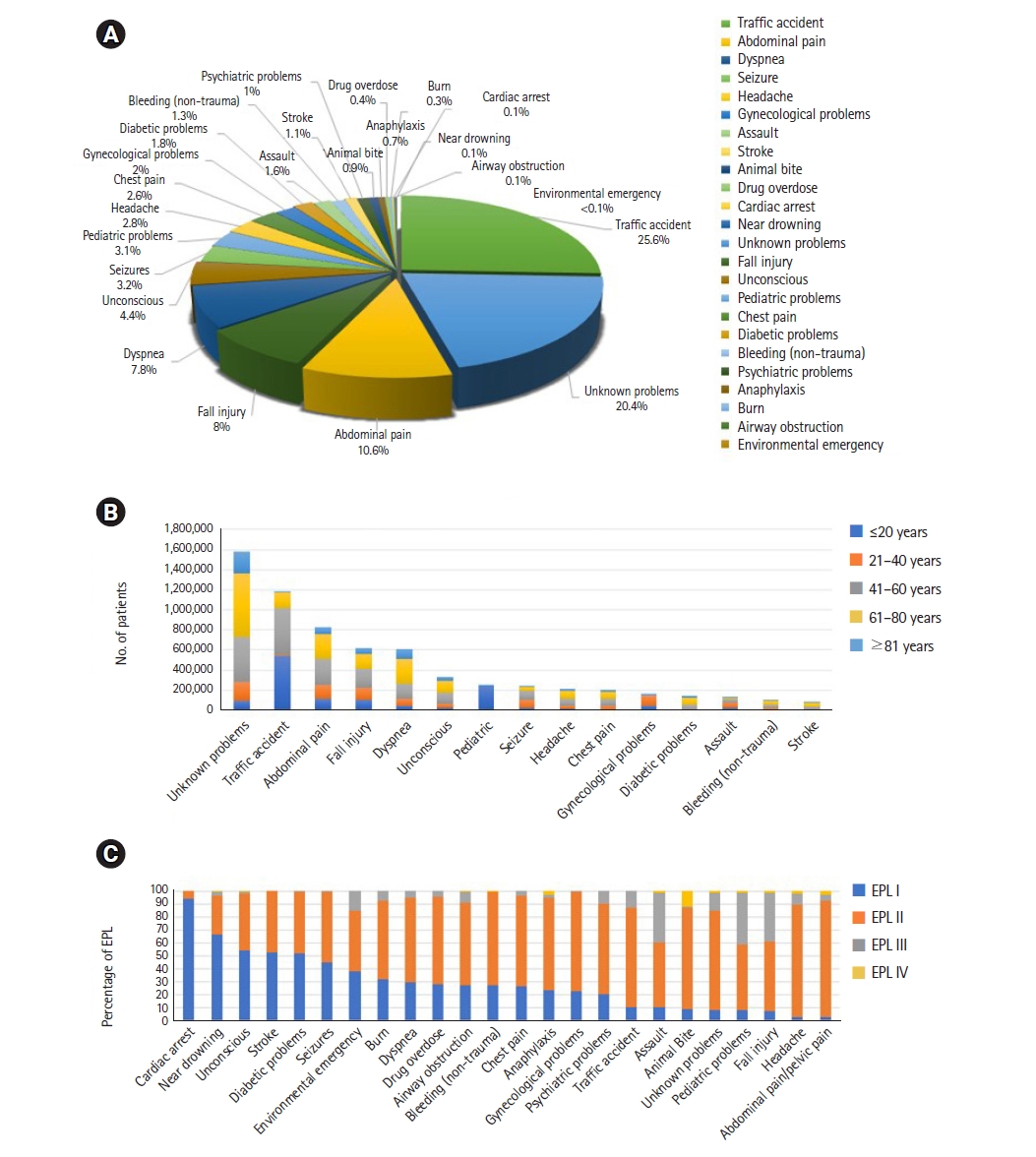
Fig. 4.

Fig. 5.
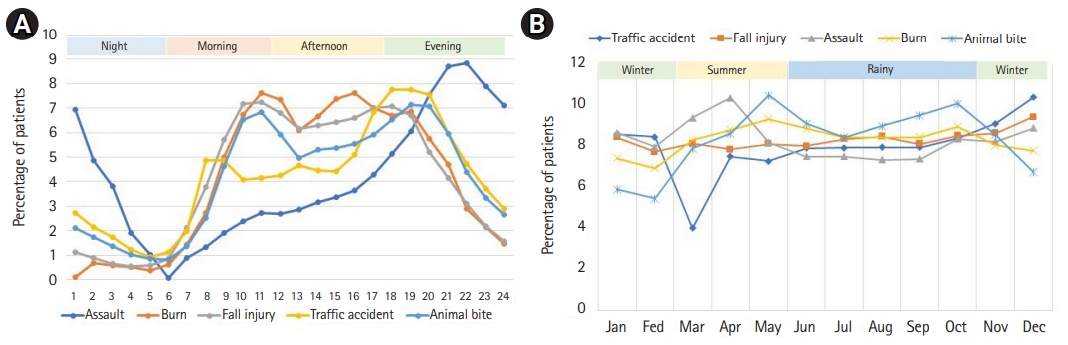
Table 1.
| Variable | EPL I | EPL II | EPL III | EPL IV | Total |
|---|---|---|---|---|---|
| Total | 1,229,425 (100.0) | 5,569,278 (100.0) | 972,596 (100.0) | 88,427 (100.0) | 7,859,726 (100.0) |
| Seasona) | |||||
| Winter | 427,157 (34.7) | 1,886,266 (33.9) | 326,874 (33.6) | 29,150 (33.0) | 266,9447 (34.0) |
| Summer | 292,509 (23.8) | 1,330,378 (23.9) | 229,981 (23.6) | 21,226 (24.0) | 1,874,094 (23.8) |
| Rainy | 509,759 (41.5) | 2,352,634 (42.2) | 415,741 (42.7) | 38,051 (43.0) | 3,316,185 (42.2) |
| Weekday | |||||
| Monday | 178,874 (14.5) | 819,034 (14.7) | 142,402 (14.6) | 13,200 (14.9) | 1,153,510 (14.7) |
| Tuesday | 176,093 (14.3) | 799,774 (14.4) | 138,810 (14.3) | 12,724 (14.4) | 1,127,401 (14.3) |
| Wednesday | 175,664 (14.3) | 801,745 (14.4) | 138,724 (14.3) | 12,753 (14.4) | 1,128,886 (14.4) |
| Thursday | 178,643 (14.5) | 803,743 (14.4) | 140,304 (14.4) | 12,996 (14.7) | 1,135,686 (14.4) |
| Friday | 179,278 (14.6) | 820,231 (14.7) | 143,247 (14.7) | 12,936 (14.6) | 1,155,692 (14.7) |
| Saturday | 170,335 (13.9) | 770,213 (13.8) | 135,569 (13.9) | 12,010 (13.6) | 1,088,127 (13.8) |
| Sunday | 170,538 (13.9) | 754,538 (13.5) | 133,540 (13.7) | 11,808 (13.4) | 1,070,424 (13.6) |
| Time of dayb) | |||||
| Night | 144,031 (11.7) | 576,381 (10.3) | 86,151 (8.9) | 8,266 (9.3) | 814,829 (10.4) |
| Morning | 358,279 (29.1) | 1,646,286 (29.6) | 283,531 (29.2) | 27,480 (31.1) | 2,315,576 (29.5) |
| Afternoon | 397,878 (32.4) | 1,822,969 (32.7) | 326,241 (33.5) | 27,958 (31.6) | 2,575,046 (32.8) |
| Evening | 329,237 (26.8) | 1,523,642 (27.4) | 276,673 (28.4) | 24,723 (28.0) | 2,154,275 (27.4) |
Values are presented as number (%).
EPLs, emergency priority levels; EPL I, red response (potentially life-threatening); EPL II, yellow response (acute, but not life-threatening); EPL III, green response (not acute, but transportation and observation in ambulance are necessary); EPL IV, white response (advise, recommendation, referral to general practitioner).