|
 |
- Search
| J EMS Med > Volume 2(1); 2023 > Article |
|
Abstract
Objective
The survival of out-of-hospital cardiac arrest (OHCA) patients depends on early bystander chest compression and rapid public access defibrillation. This study aimed to design and develop a smartphone application for bystander cardiopulmonary resuscitation (BCPR) in a prehospital setting in Thailand.
Methods
The four steps of the study were planning, development, evaluation, and production of applications through online meetings and submission of a linked questionnaire to 19 experts for consensus.
Results
Among the total of 19 experts, 93% strongly agreed with the development of the smartphone application. They agreed with the operating modes as follows: 100% with emergency calls by number and video calls, 100% with dispatchers and bystanders to locate OHCA and automated external defibrillator (AED), 94% with teaching of BCPR by video, 88% with pediatric cardiopulmonary resuscitation (CPR), 100% with tracking of real-time feedback to BCPR by voice, 88% with contacting bystanders by phone number, 83% with applications that can transmit signals from OHCA to nearby bystanders within 400 m, and 89% with first aid for daily life. Consequently, the application’s main operating modes are emergency calls, identification of OHCA and AED locations, responder call, and first aid.
Out-of-hospital cardiac arrest (OHCA) is a leading cause of global mortality [1]. The incidence rate is 50 to 60 per 100,000 person-years [2] and is comparable throughout numerous parts of the world [3,4]. In Asia Pacific, the reported OHCA is 8.2% patients with the return of spontaneous circulation (ROSC) at scene or care in transport, whereas the OHCA survival rate is 5.4% [5]. Meanwhile, Thailand shows the incidence of OHCA rate of 6,450 per year [6]. The most common location of OHCA is home residence (61.8%) [7]. The most common etiology of cardiac arrest consists of 54% presumed cardiac etiology [7]. OHCA accounts for 15.8% of compression-only bystander cardiopulmonary resuscitation (BCPR) cases in Bangkok [7]. However, Thailand reported 25.9% ROSC [5]; the outcomes showed that 27.7% of patients survived to admission, and 4.2% survived to discharge [7].
The effect of BCPR resulted in a 31.4% increase in survival [8]. Early BCPR, which is performed before the arrival of ambulance services, is one of the most significant predictors of survival after OHCA [9,10]. Early defibrillation by an automated external defibrillator (AED) and the initiation of BCPR are critical to improving the outcomes after OHCA [11]. Early defibrillations within 3 to 5 minutes of collapse can produce a survival rate of as high as 50% to 70% [12]. Each minute of delay to defibrillation reduces the probability of survival to hospital discharge by 10.7% [13]. Currently, less than 2% of OHCA patients are equipped with an AED before the ambulance arrives [14]. Using mobile technology to improve communication with the ever-growing number of mobile devices, the United States is rapidly updating their 9-1-1 service by providing better caller location information and enabling the public to transmit text, images, video, and data [15]. Adding a locator system further reduces the response time after a call from a mobile phone [16]. Using such maps, modern smartphones can help bystanders locate and retrieve nearby AEDs swiftly [15]. Recently, a published study demonstrated that the mobile AED map significantly shortened travel distances to find and retrieve AEDs [5]. Telephone cardiopulmonary resuscitation (TCPR) is independently associated with the improved survival (odds ratio [OR] 1.64, 95% confidence interval [CI] 1.16-2.30) and good neurologic outcome (OR 1.56, 95% CI 1.06-2.31) after OHCA [17]. Stroop et al. [18] reported that the survival to hospital discharge and good neurologic outcome were both increased significantly compared with conventional emergency medical service (EMS)-initiated CPR when bystander CPR was performed using the mobile-phone-based alerting system.
This study aimed to search for a method to develop and design a smartphone application for BCPR that is appropriate in the prehospital setting in Thailand.
This study was research and development toward smartphone application for BCPR in prehospital setting in Thailand.
The study was carried out from April 2020 to August 2021. The method of this study included integrated Sugiyono [19] and Delphi techniques [20,21]. Sugiyono has 4 steps: (1) planning, (2) development (validation by EMS experts and application experts, (3) evaluation, and (4) innovative product and smartphone applications for BCPR to the EMS in Thailand. Sugiyono was combined with the Delphi technique, which has 3 steps, namely, (1) identification by experts, (2) questionnaire design, and (3) measurement of consensus.
In this study, 19 experts were selected (minimize error, 0.02) [22] in EMS, including 15 emergency physicians, 3 emergency nurses, and 1 paramedic, from each region across Thailand. Then, to decide upon the questionnaire structure and appropriate rounds, we created a consensus-based questionnaire with 13 main questions and 113 sub-questions.
The main questions were the following: (1) Is the development of smartphone applications in the EMS in Thailand necessary?; (2) What do you think of the emergency call mode of activated emergency?; (3) What do you think of the dispatch center using location data?; (4) What do you think of the registered bystander who finds the location data?; (5) What do you think of the emergency medical response (EMR) use in location data?; (6) What do you think of the application being able to teach CPR for daily life?; (7) What do you think of the scope of first-aid?; (8) What do you think of the application being able to guide bystanders when providing bystander CPR?; (9) What do you think of the application being able to offer notification about real-time feedback on high-quality CPR for bystanders?; (10) What do you think of how the application gives real-time feedback to bystander CPR?; (11) What do you think of the application’s need to track bystanders to administer care?; (12) What do you think of the application’s need to track bystanders to contact?; (13) What do you think of the distance from the application to a bystander? The next step involved sending questionnaires to experts using Google forms in 2 rounds. The questionnaire focused on the 5-point Likert scale for agreement (0−5 for “do not agree” to “very much agree”). Afterward, 3 online expert meetings were held to discuss opinions and consensus (Fig. 1).
The data from the expert response to questionnaires presented as the percentage of agreement and median with interquartile ranges (IR). A combination of the 3 measures (percentage, median, interquartile range) was used, with 80% of respondents belonging to the “very important” or “strongly agree” categories. The median of the consensus assessment was more than 4, and the IRs were less than 1.5.
The 2 rounds of survey had questionnaire response rates of 94.7% (n=18) and 84.2% (n=16). The results obtained from the data showed that 93% of experts strongly agreed that application development is essential for an EMS in Thailand; 100% with emergency calls and video calls; 100% with the dispatcher, bystander, EMR being able to share the location of OHCA, nearby AED, and nearby ambulance; 94% with the teaching of CPR for daily life by video; 100% with providing a guide for BCPR by hand-only and AED; 88% with pediatric CPR; 100% with the tracking of real-time feedback to BCPR by voice; 83% with the tracking of bystanders on a given care after the case or answering the survey; 88% with contacting bystanders by phone number; 83% with the application being capable of transmitting signals of the OHCA to nearby bystanders within 400 m (Table 1).
The scope of the consensus regarding the first-aid content of the smartphone application revealed that experts strongly agreed with the scope of the first-aid content for daily life: 94% non-trauma knowledge, including airway obstruction, breathing problems, cardiac arrest, chest pain/heart problems, loss of consciousness/unconscious/syncope, seizures, or convulsions and stroke; 90% of knowledge on non-trauma practice, including allergies/stings, airway obstruction, breathing problems, cardiac arrest, unconscious/syncope, seizures or convulsions, and stroke; 86% of information on trauma knowledge, including bleeding/laceration, bone fracture/dislocation/immobilization, burns, near drowning, fall victim, spinal injury, stabbing/gunshot victim, and traffic-related injuries; 86% of data on trauma practice, including bleeding/laceration, bone fracture/dislocation/immobilization, burns, electrocution, fall victim, head injury, spinal injury, and traffic-related injuries (Table 2).
To confirm that the experts from this study strongly agreed that more than 80% of smartphone applications featured in application development are essential for EMS in Thailand, including the emergency call mode of activated emergency by number, video, and voice, the dispatch center will use the location of the OHCA, AED, bystander, and ambulance. The registered bystander can find the location of OHCA and AED. The EMR can also find the location of OHCA, AED, and ambulance. The application should be capable of teaching CPR for daily life by video, guide bystanders when they perform manual CPR via hand-only CPR, AED, and pediatric CPR; provide real-time notifications of feedback on high-quality CPR for bystanders regarding chest compression rate, chest compression depth, the recoil of chest compression, and minimize interruptions in chest compression and notifications every 2 minutes to rotate the compressor by voice. The applications need to track bystanders after care and survey by phone number. In addition, the application should be able to transmit signals of OHCA to nearby bystanders within 400 m and offer the first-aid content for daily life to 94% of the non-trauma knowledge, 90% of the non-trauma practice, 86% of the trauma knowledge, and 86% of the trauma practice (Fig. 2).
The main functions of the smartphone application under development include (1) mode of emergency call by the numbers 1669, video, and voice; (2) dispatcher, bystander, and EMR who can share location and search for OHCA, AED, and nearby ambulances; (3) CPR guide to a bystander for real-time and high-quality CPR regarding chest compression rate and depth, the recoil of chest compression, minimized interruptions in chest compression, and rotation of compressor every 2 minutes by voice; (4) tracking of bystander after the case and survey by phone number; (5) 400 m distance from the OHCA to nearby signal bystanders; (6) first-aid topics that describe knowledge and practice from 16 trauma and 13 non-trauma topics.
In a review regarding the effect of BCPR on OHCA, we observed that BCPR is the key to a linked community in the chain of survival for the immediate recognition of cardiac arrest [23]. In addition, the successful resuscitation after OHCA requires a coordinated team of advanced resuscitation and early BCPR [24]. The association with the early initiation of BCPR is critical to improving outcomes after OHCA [25]. BCPR increases the survival of OHCAs and helps OHCAs with a shockable initial rhythm [26]. Several studies have also evaluated the association between BCPR with dispatcher assistance, which is associated with improved neurological recovery [27]. The combination of public-access AED applications and BCPR increases the chance of survival by approximately four-fold in schools [25]. As a result, increased BCPR rates were associated with a 3.5-fold increase in 1-year survival [17]. Therefore, BCPR affects a number of important links in the OHCA survival chain and improves OHCA survival outcomes. In the future, we should increase BCPR training.
TCPR is independently associated with improved survival and functional outcome after OHCA [17]. The hospital discharge rates increase significantly with mobile rescuers; the patients resuscitated with a mobile rescue exhibit a good neurological outcome [18]. Patients who received TCPR also present significantly improved outcomes [28]. Telephone-assisted CPR (TA-CPR) is an influential community intervention to increasing BCPR rates [29]. BCPR rates can reach 70% to 80% in communities with well-implemented community CPR and dispatcher-initiated TCPR [17]. Using the maps from smartphones can help bystanders swiftly locate and retrieve nearby AEDs [15]. Mobile phone-based alert of nearby CPR volunteers is complementary to reducing response time and improving hospital discharge rate and neurological outcomes after OHCA [18].
Currently, smartphone applications showed an increasing influence on EMSs. Data have shown that smartphone application support decreases the response time, early access to OHCA area, immediate CPR, and early access to AED public, which will help improve the OHCA survival rate in the future.
Therefore, a smartphone application for BCPR in the prehospital setting in Thailand must be developed. Furthermore, we desire that smartphone applications will be essential and extremely helpful in the development of EMSs to increase the survival of cardiac arrest patients in Thailand.
The future model should focus on the development of smartphone applications for bystander CPR in the prehospital setting in Thailand. The features of the application should consist of 8 modes (Thai original language version): (1) Emergency SOS response: The application can make SOS calls to family members registered in advance and neighbors who have MySOS installed. (2) Basic life support guide: It will guide bystanders through the flow of basic life support utilizing OHCA. Depending on the situation, this mode can guide practices, such as chest compressions and recovery position. MySOS can also be used to request help from those who can provide assistance if necessary. In an emergency, the application offers instructions for basic first-aid and life-saving techniques. An emergency notification text message can be sent to the EMS and pre-registered emergency contacts. (3) AED/Hospital Search: Bystanders can search for nearby AEDs and hospitals on the map. The name of my present location and distance to the AED/hospital are also listed. The application can be used to verify the detailed information by tapping the list. (4) Adult/Pediatric Emergency Guide: The application can provide an idea of whether the medical condition or injury requires urgent care, or whether the situation should be monitored first and how to approach it. The recommended criteria for adults have 3 levels, which consist of emergency, urgent, and non-urgent, and 5 levels for children, including immediate, emergency, urgent, semi-urgent, and non-urgent levels. All the criteria for this determination depend on the symptoms. The content for adult emergency guide consists of difficult breathing, wheezing, asthma attack, palpitations, level of consciousness, convulsions, headache, chest pain, back pain, fever, and stomachache. The part for children’s emergency guide includes fever, convulsion, head injuries, stomachache, swallowing foreign objects, headache, vomiting, diarrheal, coughing, eye pain, ear pain, bee stings, and hiccups. (5) First-Aid Guide: This guide is based on the international consensus review paper on first-aid science with treatment recommendations published in 2020 [30]. It provides treatment methods for sudden cardiac arrest, syncope, seizures or convulsions, heart attack, stroke, anaphylaxis, airway obstruction, heatstroke, laceration/how to stop bleeding, bandage, fractured bone, head injury, spinal trauma, burns, electrocution, near drowning, dog bite, snake bite, and bee sting. (6) Medical Checkup Results: This guide includes the easy management of health examination results. The application can be used to easily manage the results of a medical examination by manually entering it or receiving data from an affiliated medical institution. The application can also be used to check for trends and year-to-year changes and values at a glance. (7) My Clinical Record: This guide is for the management of medical and health information, including medical (disease, medicine, prescription history, outpatient history, family doctor, and examination images) and health information (the number of steps, blood pressure, and weight) by linking with iOS “Health” and OMRON connect. The application can be used to manage data without manual input, and the settings can be changed anytime from [Setting]-[Health Information Cooperation]. (8) SOS Transmission: This guide can be used to easily send SOS to emergency contacts and other MySOS users nearby. The operating manual describes how to use all functions of the smartphone application (Fig. 3 shows all features of the application).
In conclusion, smartphone application mode consensus responses results have shown that 93% of experts strongly agreed with the necessity of smartphone applications, 95% with the mode of emergency calls by the number 1669, video call, and voice; 100% with dispatch centers sharing the locations of OHCA, nearby AED, a nearby hospital; 100% with bystanders being able to locate OHCA and AED, 83% with the 400 m transmission distance from the OHCA to nearby bystanders, and 94% with the first-aid content for daily life.
We designed and developed a new smartphone application for BCPR in Thailand. The next study will attempt to develop a smartphone application for training and outcome measures in Bangkok, Thailand.
ACKNOWLEDGEMENTS
FUNDING
This study was supported by the Graduate school of Emergency Medical System, Kokushikan University in Japan, Navamindradhiraj University for supporting the scholarship, National Institute for Emergency Medicine, and Thailand Science Research and Innovation for the research grant.
AUTHORS’ CONTRIBUTIONS
Conceptualization: DT; Data curation: DT; Formal analysis: DT, HT; Investigation: DT, HT; Methodology: DT, HT, TH; Project administration: DT; Resources: all authors; Software: all authors; Supervision: DT, HT; Validation: DT, HT; Visualization: DT, HT; Writing–original draft: DT, HT; Writing–review & editing: DT, HT.
Fig. 1.
Study design. OHCA, out-of-hospital cardiac arrest; App., application; IR, interquartile range; SD, standard deviation.
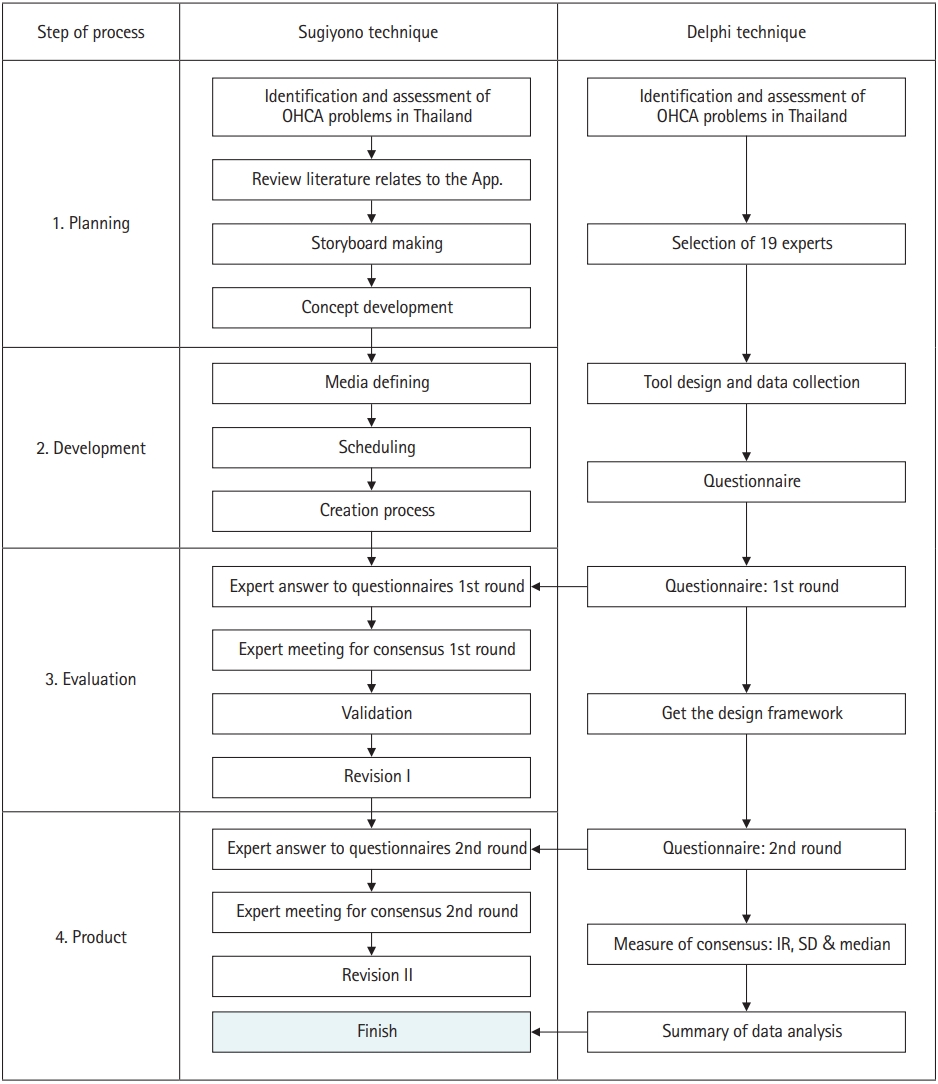
Fig. 2.
Only the features strongly agree of application mode. App., application; OHCA, out-of-hospital cardiac arrest; AED, automated external defibrillator; EMR, emergency medical response; CPR, cardiopulmonary resuscitation.
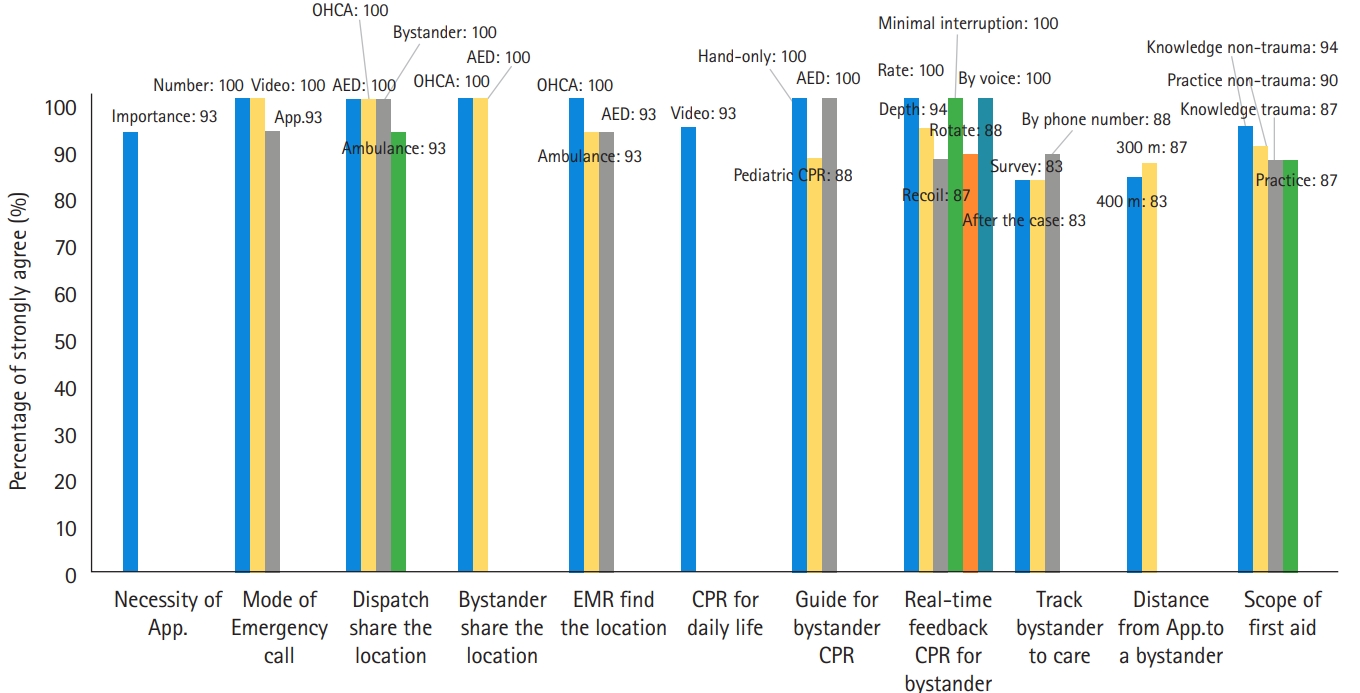
Fig. 3.
Feature for developing a smartphone application. AED, automated external defibrillator; CPR, cardiopulmonary resuscitation.
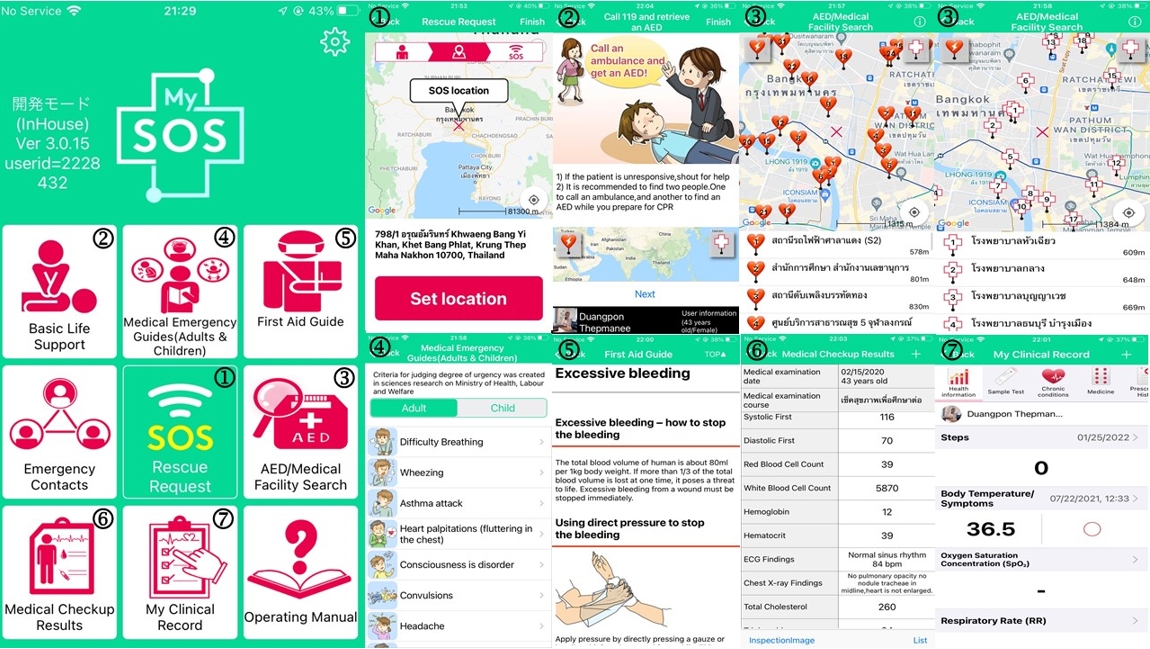
Table 1.
Consensus of the application function (n=19)
| Mode of functiona) |
% Of strong agreement |
Median |
Interquartile range |
|||
|---|---|---|---|---|---|---|
| 1st round | 2nd round | 1st round | 2nd round | 1st round | 2nd round | |
| The necessity of smartphone applications in EMS in Thailand | 88 | 93 | 5 | 4.5 | 1 | 1 |
| The emergency call mode of activating emergency rescue | ||||||
| Emergency number 1669 | 94 | 100 | 5 | 5 | 0 | 1 |
| Make video calls | 94 | 100 | 4.5 | 5 | 1 | 1 |
| Application can call | 63 | 93 | 5 | 5 | 2 | 1 |
| The dispatch center will use the location data | ||||||
| The OHCA location | 100 | 100 | 5 | 5 | 0 | 0 |
| The nearby AED location | 100 | 100 | 5 | 5 | 0 | 0 |
| The bystander nearby AED and nearby OHCA location | 94 | 100 | 5 | 5 | 0 | 1 |
| The ambulance near the OHCA location | 100 | 93 | 5 | 5 | 0 | 1 |
| The registered bystander can find the location data | ||||||
| The OHCA location | 100 | 100 | 5 | 5 | 0 | 1 |
| The AED location | 100 | 100 | 5 | 5 | 0 | 1 |
| The EMR will use the location data | ||||||
| The OHCA location | 94 | 100 | 5 | 5 | 0 | 0 |
| The nearby AED location | 88 | 93 | 5 | 5 | 1 | 1 |
| The ambulance near the OHCA location | 77 | 93 | 5 | 5 | 1 | 1 |
| To teach CPR for daily life | ||||||
| By picture | 83 | 62 | 4 | 4 | 1 | 2 |
| By text | 50 | 12 | 3.5 | 3 | 2 | 1 |
| By video | 94 | 93 | 5 | 5 | 0 | 1 |
| To guide bystander when he gives bystander CPR | ||||||
| Hands-only CPR | 88 | 100 | 5 | 5 | 0 | 0.5 |
| Conventional CPR | 50 | 56 | 3.5 | 4 | 2 | 1 |
| Pediatric CPR | 88 | 87 | 5 | 4.5 | 1 | 1 |
| Infant CPR | 72 | 82 | 4 | 4 | 2 | 0.5 |
| AED | 94 | 100 | 5 | 5 | 0 | 0 |
| COVID-19 of personal protective equipment | 66 | 75 | 5 | 4 | 1 | 1.5 |
| To notify real-time feedback of high-quality CPR for bystanders | ||||||
| Rate of chest compression | 100 | 94 | 5 | 5 | 1 | 0.5 |
| Compression depth | 94 | 94 | 5 | 5 | 1 | 0.5 |
| Recoil of chest compression | 94 | 87 | 5 | 5 | 1 | 1 |
| Interruptions in chest compressions | 100 | 94 | 5 | 5 | 1 | 0.5 |
| Notify every 2 min to rotate compressor | 88 | 81 | 5 | 5 | 1 | 1 |
| Track real-time feedback to bystander CPR | ||||||
| By light | 50 | 62 | 4 | 4 | 2 | 2 |
| By picture | 44 | 37 | 3 | 3 | 1 | 1 |
| By text | 11 | 69 | 3 | 3 | 1 | 1.5 |
| By waveform | 55 | 62 | 4 | 4 | 3 | 1 |
| By voice | 100 | 87 | 5 | 5 | 1 | 1 |
| Track bystanders on given care | ||||||
| After the case | 83 | 75 | 4 | 4 | 1 | 1.5 |
| Answer the survey | 83 | 81 | 4 | 4 | 1 | 0 |
| Contact bystanders | ||||||
| By email | 72 | 44 | 3.5 | 3 | 1 | 1 |
| By line | 61 | 75 | 4 | 4 | 1 | 1.5 |
| By phone number | 88 | 87 | 4 | 4 | 1 | 1 |
| By ID | 44 | 37 | 3 | 3 | 1 | 1 |
| The distance from applications to a bystander | ||||||
| 100 m | 61 | 81 | 4 | 5 | 1 | 1 |
| 200 m | 77 | 75 | 4 | 5 | 1 | 1 |
| 300 m | 66 | 87 | 4 | 5 | 2 | 1 |
| 400 m | 83 | 75 | 4 | 4 | 1 | 1 |
| 500 m | 77 | 69 | 4 | 4 | 1 | 2 |
Table 2.
Scope of first-aid for bystander (n=19)
| Scope of first-aid for bystandera) |
Knowledge |
Practice |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
% Of expert who agreed |
Median |
Interquartile range |
% Of expert who agreed |
Median |
Interquartile range |
|||||||
| 1st round | 2nd round | 1st round | 2nd round | 1st round | 2nd round | 1st round | 2nd round | 1st round | 2nd round | 1st round | 2nd round | |
| Non-trauma | ||||||||||||
| 1. Abdominal pain | 44 | 25 | 3 | 3 | 1.0 | 0.5 | 38 | 25 | 3 | 3 | 2.0 | 1.0 |
| 2. Allergies/stings | 72 | 81 | 5 | 4 | 2.0 | 1.0 | 83 | 75 | 5 | 4 | 1.0 | 1.0 |
| 3. Airway obstruction | 94 | 93 | 5 | 5 | 1.0 | 1.0 | 94 | 81 | 5 | 5 | 1.0 | 1.0 |
| 4. Back pain | 33 | 33 | 3 | 3 | 2.0 | 1.0 | 38 | 25 | 3 | 3 | 2.0 | 1.0 |
| 5. Breathing problems | 94 | 25 | 5 | 5 | 1.0 | 1.0 | 94 | 81 | 5 | 4.5 | 1.0 | 1.0 |
| 6. Cardiac arrest | 94 | 93 | 5 | 5 | 0.0 | 0.0 | 94 | 81 | 5 | 5 | 0.0 | 1.0 |
| 7. Chest pain/heart problems | 88 | 93 | 5 | 5 | 1.0 | 1.0 | 94 | 75 | 4 | 5 | 1.0 | 1.0 |
| 8. COVID-19 | 55 | 75 | 4 | 5 | 2.0 | 1.0 | 72 | 62 | 4 | 4 | 1.0 | 1.5 |
| 9. Diabetic problems | 50 | 62 | 3.5 | 4 | 2.0 | 1.5 | 66 | 50 | 4 | 4 | 2.0 | 1.0 |
| 10. Drug overdose/poisonings/ingestions | 61 | 75 | 4 | 4 | 2.0 | 1.5 | 72 | 62 | 4 | 4 | 2.0 | 1.0 |
| 11. Dyspnea | 72 | 93 | 4 | 4 | 2.0 | 1.0 | 72 | 69 | 4.5 | 4 | 2.0 | 1.0 |
| 12. Headache | 50 | 37 | 3.5 | 3 | 1.0 | 1.0 | 55 | 56 | 3 | 3 | 1.0 | 2.0 |
| 13. Loss of consciousness/unconscious/syncope | 94 | 87 | 5 | 5 | 0.0 | 1.0 | 94 | 69 | 5 | 5 | 1.0 | 1.0 |
| 14. Pregnancy/gynecological problems | 55 | 50 | 4 | 3.5 | 1.0 | 1.5 | 66 | 44 | 3.5 | 4 | 1.0 | 1.5 |
| 15. Psychiatric/behavioral problems | 44 | 56 | 3 | 4 | 1.0 | 1.5 | 61 | 50 | 3.5 | 4 | 1.0 | 1.0 |
| 16. Seizures or convulsions | 94 | 87 | 5 | 5 | 1.0 | 1.0 | 83 | 69 | 5 | 4 | 1.0 | 1.0 |
| 17. Stroke | 94 | 93 | 5 | 5 | 0.0 | 1.0 | 83 | 69 | 5 | 4 | 1.0 | 2.0 |
| Trauma | ||||||||||||
| 1. Animal bite or bee sting | 77 | 69 | 4 | 4 | 1.0 | 1.0 | 77 | 69 | 4 | 4.5 | 1.0 | 2.0 |
| 2. Assault/violence/sexual assault | 61 | 62 | 4 | 5 | 1.0 | 1.0 | 27 | 62 | 4 | 4 | 1.0 | 2.0 |
| 3. Bleeding/laceration | 88 | 81 | 5 | 4 | 1.0 | 1.0 | 94 | 44 | 5 | 5 | 1.0 | 0.5 |
| 4. Broken bone/dislocation/immobilization | 94 | 81 | 5 | 4 | 0.0 | 1.0 | 88 | 87 | 5 | 5 | 1.0 | 1.0 |
| 5. Burns | 83 | 81 | 5 | 3 | 1.0 | 1.0 | 83 | 75 | 5 | 5 | 1.0 | 1.5 |
| 6. Cold exposure | 61 | 44 | 4 | 4 | 1.0 | 1.0 | 50 | 37 | 3.5 | 3 | 2.0 | 1.0 |
| 7. Near drowning | 88 | 94 | 5 | 4.5 | 2.0 | 1.0 | 55 | 94 | 5 | 5 | 1.0 | 1.0 |
| 8. Electrocution | 83 | 75 | 5 | 4 | 1.0 | 1.5 | 88 | 81 | 5 | 4.5 | 1.0 | 1.0 |
| 9. Eye injuries | 55 | 55 | 4 | 4 | 1.0 | 1.0 | 61 | 75 | 4 | 4 | 2.0 | 1.5 |
| 10. Fall victim | 83 | 75 | 4 | 4.5 | 2.0 | 1.0 | 83 | 75 | 4 | 4 | 1.0 | 1.0 |
| 11. Head injury | 77 | 75 | 5 | 4 | 1.0 | 1.0 | 83 | 87 | 4.5 | 4.5 | 1.0 | 1.0 |
| 12. Heat exposure | 83 | 75 | 4 | 4.5 | 1.0 | 2.0 | 66 | 81 | 4 | 4 | 2.0 | 1.0 |
| 13. Spinal injury | 88 | 75 | 5 | 5 | 1.0 | 1.0 | 83 | 87 | 4 | 5 | 1.0 | 1.0 |
| 14. Stabbing/gunshot victim | 83 | 75 | 5 | 5 | 1.0 | 1.5 | 72 | 81 | 4 | 4.5 | 1.0 | 1.0 |
| 15. Traffic-related injuries | 77 | 87 | 5 | 4 | 1.0 | 1.0 | 88 | 87 | 4 | 4 | 1.0 | 1.0 |
REFERENCES
2. Doctor NE, Ahmad NS, Pek PP, Yap S, Ong ME. The Pan-Asian Resuscitation Outcomes Study (PAROS) clinical research network: what, where, why and how. Singapore Med J 2017;58:456–8.



3. Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics: 2015 update: a report from the American Heart Association. Circulation 2015;131:e29–322.


4. Kleinman ME, Brennan EE, Goldberger ZD, et al. Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015;132(18 Suppl 2):S414–35.

5. Liu N, Ong ME, Ho AF, et al. Validation of the ROSC after cardiac arrest (RACA) score in Pan-Asian out-of-hospital cardiac arrest patients. Resuscitation 2020;149:53–9.


6. Khuhakan R, Chusang S, Somton A, Suwannarak U, Suwannarak S. Report on the situation of the Thai emergency medical system. Bangkok: National Institute for Emergency Medicine; 2016.
7. Ong ME, Shin SD, De Souza NN, et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: the Pan Asian Resuscitation Outcomes Study (PAROS). Resuscitation 2015;96:100–8.


8. Baldi E, Caputo ML, Savastano S, et al. An Utstein-based model score to predict survival to hospital admission: the UB-ROSC score. Int J Cardiol 2020;308:84–9.


9. Viereck S, Palsgaard Moller T, Kjaer Ersboll A, Folke F, Lippert F. Effect of bystander CPR initiation prior to the emergency call on ROSC and 30day survival: an evaluation of 548 emergency calls. Resuscitation 2017;111:55–61.


10. Hasselqvist-Ax I, Riva G, Herlitz J, et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med 2015;372:2307–15.


11. Pollack RA, Brown SP, Rea T, et al. Impact of bystander automated external defibrillator use on survival and functional outcomes in shockable observed public cardiac arrests. Circulation 2018;137:2104–13.



12. Mendelson J, Berg MD. Getting the right bystander to the right place at the right time. Resuscitation 2016;107:A11–2.


13. Rajan S, Wissenberg M, Folke F, et al. Association of bystander cardiopulmonary resuscitation and survival according to ambulance response times after out-of-hospital cardiac arrest. Circulation 2016;134:2095–104.


14. Berglund E, Claesson A, Nordberg P, et al. A smartphone application for dispatch of lay responders to out-of-hospital cardiac arrests. Resuscitation 2018;126:160–5.


16. Caputo ML, Muschietti S, Burkart R, et al. Lay persons alerted by mobile application system initiate earlier cardio-pulmonary resuscitation: a comparison with SMS-based system notification. Resuscitation 2017;114:73–8.


17. Wu Z, Panczyk M, Spaite DW, et al. Telephone cardiopulmonary resuscitation is independently associated with improved survival and improved functional outcome after out-of-hospital cardiac arrest. Resuscitation 2018;122:135–40.


18. Stroop R, Kerner T, Strickmann B, Hensel M. Mobile phone-based alerting of CPR-trained volunteers simultaneously with the ambulance can reduce the resuscitation-free interval and improve outcome after out-of-hospital cardiac arrest: a German, population-based cohort study. Resuscitation 2020;147:57–64.


19. Sugiyono. Metode Penelitian Kuantitatif, Kualitatif, dan R&D. Bandung: Alfabeta; 2015.
20. Giannarou L, Zervas E. Using Delphi technique to build consensus in practice. Int J Bus Sci Appl Manag 2014;9:65–82.
21. Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval 2007;12:10.
23. Viereck S, Moller TP, Ersboll AK, et al. Recognising out-of-hospital cardiac arrest during emergency calls increases bystander cardiopulmonary resuscitation and survival. Resuscitation 2017;115:141–7.


24. Kronick SL, Kurz MC, Lin S, et al. Part 4: systems of care and continuous quality improvement: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015;132(18 Suppl 2):S397–413.

25. Kiyohara K, Sado J, Kitamura T, et al. Public-access automated external defibrillation and bystander-initiated cardiopulmonary resuscitation in schools: a nationwide investigation in Japan. Europace 2019;21:451–8.


26. Song J, Guo W, Lu X, Kang X, Song Y, Gong D. The effect of bystander cardiopulmonary resuscitation on the survival of out-of-hospital cardiac arrests: a systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med 2018;26:86.



27. Ro YS, Shin SD, Song KJ, et al. Effects of dispatcher-assisted cardiopulmonary resuscitation on survival outcomes in infants, children, and adolescents with out-of-hospital cardiac arrests. Resuscitation 2016;108:20–6.


28. Shibahashi K, Ishida T, Kuwahara Y, Sugiyama K, Hamabe Y. Effects of dispatcher-initiated telephone cardiopulmonary resuscitation after out-of-hospital cardiac arrest: a nationwide, population-based, cohort study. Resuscitation 2019;144:6–14.